- Visibility 69 Views
- Downloads 11 Downloads
- DOI 10.18231/j.ijashnb.2020.027
-
CrossMark
- Citation
Frontal sinus inverted papilloma: Osteoplastic flap approach
- Author Details:
-
Abhimanyu Kadapathri *
-
K C Prasad
-
S M Azeem Mohiyuddin
-
Pradeep Krishna
-
Priyanka Das
Introduction
Inverted papilloma is a benign neoplasm of epithelial ingrowth into the underlying stroma. Predominantly common in sino-nasal area with relatively rare incidence in frontal sinus when compared to other areas. It is known for its invasiveness, tendency to recur and chances of malignant transformation.[1], [2] The first described documentation of inverted papilloma is by Ward in 1854.[3] Hyams later subdivided this tumor into inverted, fungiform and cylindrical types.[4] Management of these neoplasms in frontal sinus pose a great challenge to rhinologists. The tight anatomical boundaries and limitations in instrumentation further curbs access to these tumors even in this modern age of endo-nasal surgery. Endoscopic access is restricted in tumors which are laterally and superiorly placed. Osteoplastic flap technique devised by Goodwin and Montgomery could address these issues not amenable for endoscopic surgery. [5]
Case Report
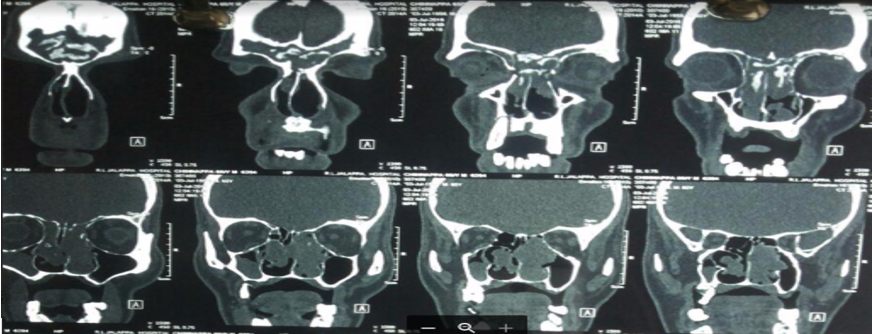
A 55 year old male patient has presented to us with complaints of unilateral nasal obstruction, hyposmia and recurrent fronto-temporal headache since 9 years. He also gave a history of worsening of these symptoms since past 6 months. Patient gave history of undergoing multiple endo-nasal surgeries in the past, for which details were not available. On endoscopic examination pinkish, pedunculated, irregular, firm mass was located filling space lateral to bilateral middle turbinates and right nasal cavity. On probing, mass was felt attached to lateral walls and superiorly in both nasal cavities and mass did not bleed on touch. Computed tomography (CT) scan was advised and it revealed that the tumor was filling bilateral frontal sinuses, right maxillary sinus with widening of osteo-meatal complex. On contrast, there was mild to moderate enhancement seen in the tumor. This mass was quite large and there were multiple erosions seen in frontal sinus walls. ([Figure 1]) We performed a biopsy of this lesion. Based on the clinical features, histopathologic features and radiographic findings, a provisional diagnosis of an inverted papilloma was given. After an adequate workup and informed consent, patient was planned for a combined approach excision with an osteoplastic flap. We have approached neurosurgery colleagues for assistance and evaluation.
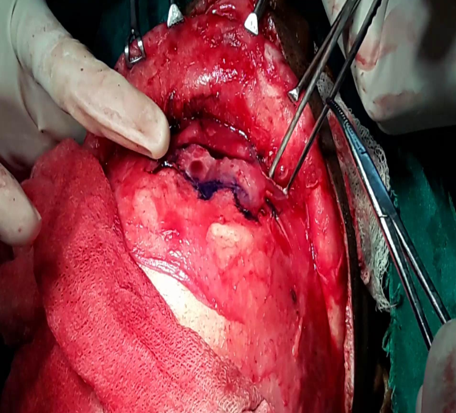
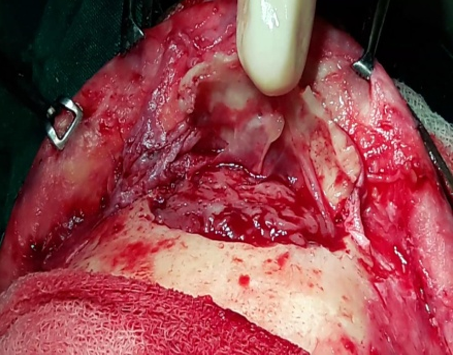
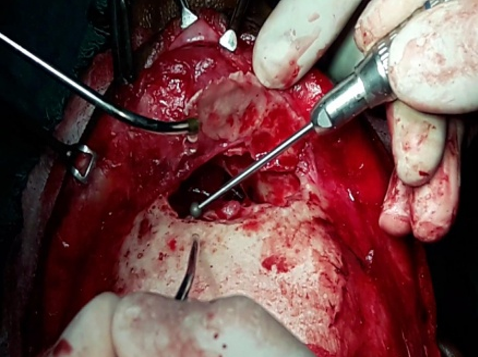
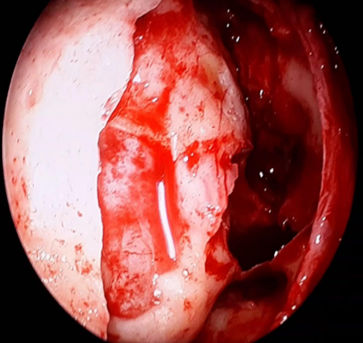
Under hypotensive general anaesthesia, patient was positioned for endoscopic sinus surgery and tumor debulking was performed. Tumor tissue was sent for frozen section confirmation to rule out malignancy. Draf type III frontal sinusotomy with right sided medial maxillectomy was performed. A sterilized template was cut out for frontal sinus exposure using a 6 feet Caldwell view radiograph ([Figure 2]). A bi coronal incision was taken after adequate preparation of scalp, anterior scalp flap was raised anteriorly till supra-orbital ridge. Galeal- Pericranial flap was based anteriorly and fashioned appropriately expecting there may be a need for duraplasty. A powered drill was used to make the osteotomy along the presumed contours of frontal sinus using the template ([Figure 3]), taking care of not damaging pericranial flap. Upon exposure tumor in the frontal sinuses was slowly taken out. Few breaches in frontal sinus posterior wall were examined for dural tear and cerebro spinal fluid leak. All walls of frontal sinus are meticulously drilled with a diamond burr ([Figure 4]). As no cerebro spinal fluid leak or no major posterior wall breach was found, we abandoned cranialisation of frontal sinus. Bone wax was used for hemostasis. Adequate sterility was followed throughout the procedure. Sinus cavity was packed with antibiotic impregnated sterile gelfoam. Adequacy of frontal sinus drainage and tumor clearance was further conformed under endoscopic assistance endo-nasally and from cranial end ([Figure 5]). Bone flap was repositioned and secured with titanium miniplates. Pericranial flap was always kept attached to the bone flap to maintain its blood supply. Both nasal cavities were packed with Sterile nasal packs and antibiotic ointment. Post operatively patient was extubated after the procedure and monitored overnight in intensive care unit. Patient was moved to ward on postoperative day one. Nasal packs were removed 24 hours post procedure. Patient was discharged on postoperative day four.
Discussion
Inverted papilloma was defined as a group of benign neoplasms arising from Schneiderian (sino-nasal) mucosa. Amongst papillomas of sinonasal region, inverted papilloma is the most common and oncocytic variant is the least common. [6] Inverted papillomas usually occur along the lateral nasal wall (middle turbinate or ethmoid recesses), with secondary extension into the paranasal sinuses. They generally originate in paranasal sinus with/without involving nasal cavity. Typically, schneiderian papillomas are unilateral; bilateral papillomas may also occur.
External approach in this modern age of endonasal endoscopic surgery is limited to only about 5% of all frontal sinus surgeries. [7] There are various surgical approaches described in literature to deal with frontal sinus disorders can be either external, intranasal, or combined depending on the type and extent of disease. Availability of such a wide variety of treatment modalities makes the optimal management protocol for frontal sinus disorders a matter of debate. In addition, no single approach has been able to fulfill the criteria for the modality of choice in terms of excellent results, no recurrence or residual disease, minimal morbidity, short hospital stay, uneventful long-term postoperative course, and good cosmesis in cases of extensive disease and extrasinus involvement. Pietroban G [8] has proposed a practical algorithm for treatment planning based on the extent of frontal sinus involvement. He proposed the use of osteoplastic flap approach combined with endoscopic approach in situations as follows.
Attachment to anterior wall or upper half posterior wall
Small antero-posterior diameter
Short interorbital distance
Massive frontal sinus involvement
Lateral supraorbital attachment in laterally pneumatized sinus
Scar tissue and anatomic distortion from previous surgeries
Krouse [9] has proposed a staging system for inverted papillomas which is widely used by surgeons, which is depicted in[Table 1].
| T1 | Confined to nasal cavity, without extension into paranasal sinuses and can be localized to one wall or region of nasal cavity |
| T2 | Involves osteomeatal complex and ethmoids and/or medial portion of maxillary sinus, sphenoid sinus and/or nasal cavity |
| T3 | Involving sphenoid and/or frontal sinus and/or lateral,superior, anterior or posterior walls of maxillary sinus |
| T4 | Extra nasal or extrasinus extension and/or tumours associated with malignancy |
Complications of osteoplastic approach includes accidental fracture or misplacement of anterior table of frontal sinus, accidental breach into cranium, cerebrospinal fluid leak, scarring of skin, osteomyelitis, contour abnormalities, frontal anesthesia and supraorbital nerve neuralgia. [10]
Conclusion
Osteoplastic bone flap procedure is one of the most relevant external approaches to frontal sinus surgery even today. While more emphasis is being given to endoscopic approaches in the present era, osteoplastic flap approach still needs to be a part of the teaching curriculum and surgeons armamentarium keeping in mind its cost-effectiveness, with almost no need for a specialized infrastructure and the relative ease for beginners. Osteoplastic flap technique is thus here to stay until the time endoscopic setup and navigation system is widespread in every level of healthcare delivery system.
Source of Funding
None.
Conflict of Interest
None.
References
- C T Melroy, B A Senior. Benign Sinonasal Neoplasms: A Focus on Inverting Papilloma. Otolaryngol Clin North Am 2006. [Google Scholar]
- J K Han, T L Smith, T Loehrl, R J Toohill, M M Smith. An Evolution in the Management of Sinonasal Inverting Papilloma. Laryngoscope 2001. [Google Scholar]
- N Ward. A mirror of the practice of medicine and surgery in the hospitals of London. London Hosp Lancet 1854. [Google Scholar]
- Vincent J. Hyams. Papillomas of the Nasal Cavity and Paranasal Sinuses. Ann Otol, Rhinol Laryngol 1971. [Google Scholar]
- R. L. Goodale, W. W. Montgomery. LXV Anterior Osteoplastic Frontal Sinus Operation. Ann Otol, Rhinol Laryngol 1961. [Google Scholar]
- W Lawson, Le Benger, J Som, P Bernard, P J Biller, H F. Inverted papilloma: An analysis of 87 cases. Laryngoscope 1989. [Google Scholar]
- U Bockmuhl, S E Kountakis, B A Senior, Kountakis SE, Senior A, Draf W. Wolfgang Draf osteoplastic frontal sinusotomy and reconstruction of frontal defects. Frontal sinus stilianos, thieme 2005. [Google Scholar]
- G. Pietrobon, A. Karligkiotis, M. Turri-Zanoni, E. Fazio, P. Battaglia, M. Bignami. Surgical management of inverted papilloma involving the frontal sinus: a practical algorithm for treatment planning. Acta Otorhinolaryngologica Ital 2019. [Google Scholar]
- J H Krouse. Development of a Staging System for Inverted Papilloma. Laryngoscope 2000. [Google Scholar]
- W Lawson, A J Reino. Management of Embossment Following the Frontal Osteoplastic Operation. Laryngoscope 1996. [Google Scholar]
