- Visibility 92 Views
- Downloads 13 Downloads
- DOI 10.18231/j.ijashnb.2020.028
-
CrossMark
- Citation
Ameloblastic carcinoma: A case series, including a case with pulmonary metastasectomy
- Author Details:
-
Abhimanyu Kadapathri *
-
Ashwini Munnangi
-
Vijay Pillai
-
Vidya Vidya
-
Vivek Shetty
Introduction
Odontogenic malignancy is an extremely rare entity reported in the literature for over a hundred years.[1], [2] In 1972, the World Health Organization (WHO) classification of odontogenic malignant neoplasms included an entity called malignant ameloblastoma. [3] The term ameloblastic carcinoma was introduced by Elzay [4] in 1982 and suggested a modified classification. The rationale was that ameloblastic carcinoma has histological signs of malignancy while malignant ameloblastoma retains its benign ameloblastoma features at the metastatic site. Slootweg and Muller [5] in 1984 have further recommended amendments in WHO classification. It is only in 2005 WHO update [6] ameloblastic carcinoma was included under malignant ameloblastoma and it was further subdivided into primary type (develops de novo) and secondary type (malignant transformation of ameloblastoma). The secondary variant was further subdivided into intraosseous and peripheral variants. In the 2017 WHO classification, ameloblastic carcinoma was placed under malignant ameloblastoma without further subdivisions while metastasizing ameloblastoma along with other benign entities was placed under the heading- benign ameloblastoma. [7] These malignant variants tend to metastasize to lungs in 75% cases, which is the most common site, followed by bone, liver and brain in decreasing incidence. Literature reports a median time interval from initial treatment to distant metastases of about 9-18 years. [8], [9] The mainstay treatment for these tumours is surgical resection with wide margins(2-3 cm) with an appropriate mandibulectomy or maxillectomy. [10] There is no level 1 evidence till date for addressing neck in clinically and radiologically node-negative necks and administration of adjuvant chemotherapy, radiation or both.
Case 1
A 14-year-old male patient presented to our department with swelling in the left upper alveolus, He gave a history of slow increase in size for 5 years with a history of loosening of teeth. He underwent a biopsy elsewhere reported to be ameloblastic carcinoma. We have reviewed the histopathological diagnosis with a repeat biopsy and advised a contrast-enhanced computed tomography scan including head, neck and chest regions to rule out any metastases. The case was discussed in the multidisciplinary tumour board and surgery with curative intent was planned. The patient underwent a partial maxillectomy and selective neck dissection I-IV and defect reconstructed with fibula free flap and primary dental implants. The postoperative stay was uneventful for the patient. Final histopathology was ameloblastic carcinoma which showed hyperplastic epithelium arranged in the form of trabeculae /plexiform with peripheral columnar cells and central stellate reticulum like cells. Tall columnar cells showed palisaded nuclei, stratification, mild nuclear pleomorphism and clear cytoplasm. There was no evidence of necrosis. The cystic cavity of the tooth (impacted 3rd molar) showed odontogenic epithelial cell rests with a focus of invasive tumour. All mucosal, bony and soft tissue margins were at least 5 mm away. No lymphovascular or perineural invasion was seen. All 46 lymph nodes dissected were free of tumour. The patient was given an option of postoperative radiotherapy, which he did not opt for. He was on close follow up for 88 months till now and did not show any signs of disease on follow up scans.
Case 2
A 23-year-old lady came with complaints of swelling on the right side of the jaw for 4 months. She had undergone a biopsy elsewhere which was reported as ameloblastic carcinoma. Slide review with an onco-pathologist at our centre was confirmatory of the previous diagnosis. She underwent segmental mandibulectomy and SND I-II with a free fibula flap reconstruction. Final histopathology showed an intraosseous tumour of 2.1x3x1.5 cm in size without extensive soft tissue invasion. Cellular tumour in island with a plexiform pattern consisting of irregular masses and cord of epithelial cells with minimal stroma, focal follicular pattern also was seen. These islands were lined by basal columnar cells in a palisading pattern with hyperchromatic nuclei and polarized away from basement membrane with suprabasal cells resembling stellate reticulum, also seen were areas of transition comprising of basaloid hyperplasia, squamous metaplasia, cells with mild pleomorphism and some with prominent nucleoli. Mitotic activity of 3-4 /10 HPF noted. No evidence of perineural invasion or lymphovascular invasion was seen. Lymph nodes were free of tumour. Her hospital stay was uneventful and got discharged by the tenth postoperative day after resuming oral diet. She underwent 33 fractions, 60 gray radiation for the primary in the form of intensity-modulated radiation therapy which was initiated 4 weeks post-surgery and completed without any treatment interruptions. 6 weeks following radiation she underwent a follow-up computed tomography scan which didn’t show any evidence of disease recurrence. She is on regular followup and had undergone secondary dental implants 1-year post-radiation, currently, she is 75 months post-surgery and disease-free.
Case 3
A 34-year-old male patient came with complaints of a non-healing ulcer on the hard palate for 1 year. The patient did not have any history of consumption of tobacco or related products. PET CT has shown a 3.5 x 4 cm mass in the left maxilla extending into infratemporal fossa with erosion of pterygoid plates. The clinical diagnosis was either a minor salivary gland tumour or extraosseous ameloblastoma or a squamous cell carcinoma. Biopsy gave a histological diagnosis of ameloblastic carcinoma. He underwent left subtotal maxillectomy sparing orbital floor with complete infratemporal fossa clearance and a selective neck dissection I-IV. Reconstruction was performed using an anterolateral thigh free flap. On final histopathology Total size of the tumour was about 3.5 x 1.8 x 3 cm and closest medial pterygoid muscle margin is 0.2 cm, there was extensive involvement of medial and lateral pterygoid muscles and maxillary bone. All 37 lymph nodes dissected were free of tumour. After discussion in the multidisciplinary tumour board, the patient was advised postoperative adjuvant radiation. He has completed 60 gray 33 fractions of radiotherapy without interruptions and is on regular follow up. Followup scan was performed 10 weeks post-radiation has come disease-free. Currently, he is 62 months post-surgery and performing well.
Case 4
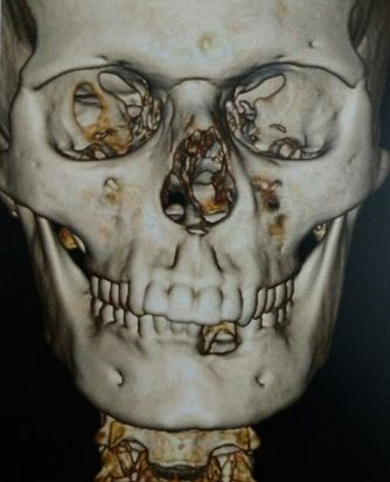
A 22-year-old patient who has already undergone multiple curettages elsewhere for a jaw lesion since 4 years has presented to us. Clinically patient had a left lower alveolus swelling with firm mass with bosselated surface and no mucosal ulceration ([Figure 1]). A biopsy report from elsewhere was descriptive of ameloblastoma. CT head, neck and chest was performed with contrast to visualize the extent of the tumour ([Figure 2]). The patient underwent segmental mandibulectomy and free iliac crest bony reconstruction and primary dental implants without neck dissection. Bony margins achieved were more than 1.5 cm, the closest margin was posterior soft tissue margin towards the lingual aspect of 0.2 cm. Final histopathology was suggestive of ameloblastic carcinoma. Postoperatively patient did not opt for adjuvant radiation and agreed on close follow up. Positron Emission Tomography (PET) scan was performed in the fifth postoperative month which showed an indeterminate solitary lung nodule of 0.8 x 0.6 cm size with SUV max of 4.7. Loco regionally there was no evidence of disease. Second follow-up scan (CT chest) was done 6 months after the first follow up scan which showed no progression in size of the lung lesion. 6 months later a PET-CT was repeated which showed a doubling of the size of the nodule with cavitation ([Figure 3]) and increased SUV max to 6.5. In view of these alarming findings, a thoracic surgeon consultation was taken and the patient underwent metastasectomy with video-assisted thoracic surgery. Intraoperatively a suspicious enlarged station IX lymph node (inferior pulmonary ligament node) was excised for sampling. The resected lung tissue showed a 1.9 x 1.2 x 1.5 cm tumour nodule consistent with ameloblastic carcinoma and the sampled lymph node showed reactive hyperplasia and no evidence of tumour. The patient did not opt for any chemotherapy and has been on close follow up since then. One year post metastasectomy PET CT showed no evidence of disease loco regionally or elsewhere in the body.


Discussion
Ameloblastic carcinoma is a very rare malignancy mainly affecting mandible and maxilla in decreasing order of incidence. Maxillary lesions occur slightly later in life compared to mandible.[11] In our case the median age was 23.25 (range 14 to 34).
Histopathological diagnosis of ameloblastic carcinoma is difficult especially when it arises denovo and it should be differentiated from primary intraosseous squamous cell carcinoma, high grade mucoepidermoid carcinoma and other metastatic carcinomas of jaw. Therefore histopathological features of ameloblastoma like peripheral palisading, reverse polarity and stellate reticulum like structure in the background of anaplasia and frequent mitotic figures provide clues in diagnosis of this entity.[12] Treatment of choice would be curative intent surgical resection with wide margins, determined by site and extent of tumour. There are a very few reports comparing surgery, radiation and chemotherapy. A systematic review of 153 cases to identify prognostic factors has shown that surgery with or without neck dissection (140.134 months, 95%CI 106.247–174.02) is the best primary modality of treatment. Radiotherapy (17.5, 95%CI 2.948–32.052) or chemotherapy (8 months, 95%CI 8 to 8) alone was not effective. The survival analysis has shown no benefit of additional treatment such as radiotherapy or chemotherapy. The extreme age groups (children, young adults and old) are more inclined to poor prognosis and survival. Categorisation of ameloblastic carcinoma into different histologic subtypes is conceptual rather than empirical.[13]
It is still unclear whether patients would be benefited with addition of adjuvant radiation and chemotherapy and impact of neck dissection in these patients. We have employed a strategy of complete surgical excision with wide margins (minimum of 2 cm) with performing selective neck dissection in case of clinically or radiologically suspected nodes. All of our cases have survived without loco regional recurrence till date. As postoperative radiation is not well established we have advised patients with extensive soft tissue involvement or close margins to undergo adjuvant radiation. Two patients have undergone Intensity Modulated Radiation Therapy (IMRT) without any treatment breaks or morbid complications. All patients resumed oral diet by 7th postoperative day and underwent dental rehabilitation either primarily or at a later date. There are few reports of use of carbon ion therapy, stereotactic radiosurgery and proton beam therapy as primary and adjuvant setting with promising results, but this area needs to be still explored.[14], [15], [16]
Metastases from ameloblastic carcinoma and metastasizing ameloblastoma usually present late after initial treatment. Usual site of metastases would be lymph nodes and lungs. Three routes commonly mentioned are hematogenous, lymphatic, and by aspiration.[17] Incidence of additional extrapulmonary metastases is less because, the pulmonary capillaries evidently provide an effective barrier for ameloblastoma cells and prevent further dissemination into the systemic circulation.[18] Multiple surgeries and curettages will increase the risk of metastases and disseminates tumour to adjacent structures.[17], [19] Case 4 had a similar history with multiple curettages and had presented with lung metastasis 5 months after primary resection. Isolated or discrete lung metastases have been treated by wedge resection or lobectomy. Resection with preservation of as much viable lung tissue as possible is the go to in isolated or resectable peripherally situated metastases.[17], [20] Chemotherapy has been used, with wide range of agents and had variable results.Only few cases showed reduction in tumour load with chemotherapy.[17], [20] Unresectable metastases should be considered for palliative radiation and chemotherapy.[17]
Conclusion
As diagnosis of ameloblastic carcinoma focus in an ameloblastoma is common, we recommend imaging to cover head, neck and chest. After adequate evaluation an early aggressive surgery would be recommended in resectable disease with a wide margin even in case of ameloblastoma, which would address the issues of recurrence in future. We recommend a margin of 2 cm for all cases of lesions which fall into ameloblastoma category. Metastatic disease should be adequately evaluated and addressed with surgery whenever possible. We would like to emphasize how important it is to maintain in contact with these patients and perform imaging in feasible intervals to identify any possible recurrence or metastases at an early stage. If addressed properly, majority of these patients would have a prolonged lifespan.
Source of Funding
None.
Conflict of Interest
None.
References
- M Emura. A case of metastatic ameloblastoma. Jap J Surg 1923. [Google Scholar]
- R F Carr, V Halperin. Malignant ameloblastomas from 1953 to 1966. Oral Surg, Oral Med, Oral Pathol 1968. [Google Scholar]
- J Pindborg, I Kramer, H Torloni. Historical Typing of Odontogenic Tumors, Jaw Cysts, and Allied Lesions. 1972. [Google Scholar]
- R P Elzay. Primary intraosseous carcinoma of the jaws. Review and update of odontogenic carcinomas. Oral Surg Oral Med Oral Pathol 1982. [Google Scholar]
- P J Slootweg, H Müller. Malignant ameloblastoma or ameloblastic carcinoma. Oral Surg, Oral Med, Oral Pathol 1984. [Google Scholar]
- L Barnes, J W Eveson, P Reichart, D Sidransky. World Health Organization Classification of Tumours: Pathology and Genetics of Head and Neck Tumors. 2005. [Google Scholar]
- A K El-Naggar, J K C Chan, J R Grandis, Takashi Takata. Fourth edition - WHO - OMS -. in IARC, Lyon WHO classification of tumours of the oral cavity. Classification of Head and Neck Tumours 2017. [Google Scholar]
- E H Laughlin. Metastasizing ameloblastoma. Cancer 1989. [Google Scholar]
- S D Van Dam, K K Unni, E E Keller. Metastasizing (Malignant) Ameloblastoma: Review of a Unique Histopathologic Entity and Report of Mayo Clinic Experience. J Oral Maxillofac Surg 2010. [Google Scholar]
- W M Mendenhall, J W Werning, R Fernandes, R S Malyapa, N P Mendenhall. Ameloblastoma. Am J Clin Oncol 2007. [Google Scholar]
- K Dhir, J Sciubba, R P Tufano. Ameloblastic carcinoma of the maxilla. Oral Oncol 2003. [Google Scholar]
- H J Yoon, S P Hong, J I Lee. Ameloblastic carcinoma: an analysis of 6 cases with review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009. [Google Scholar]
- T S Saluja, R Hosalkar. Reconnoitre ameloblastic carcinoma: A prognostic update. Oral Oncol 2018. [Google Scholar]
- A D Jensen, S Ecker, M Ellerbrock, A Nikoghosyan, J Debus, M W Münter. Carbon ion therapy for ameloblastic carcinoma. Radiat Oncol 2011. [Google Scholar]
- Y Takahashi, N Bandoh, A Miyamoto, H Kamada. Single-Fraction Helical Tomotherapy for Ameloblastic Carcinoma. J Oral Maxillofac Surg 2016. [Google Scholar]
- K Yamagata, H Ishikawa, T Saito, H Bukawa. Proton Beam Therapy for Ameloblastic Carcinoma of the Maxilla: Report of a Rare Case. J Oral Maxillofac Surg 2019. [Google Scholar]
- J M Henderson, J R Sonnet, C Schlesinger, R Ord. Pulmonary metastasis of ameloblastoma: Case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999. [Google Scholar]
- E Kunze, K Donath, H G Luhr, W Engelhardt, R. De Vivie. Biology of Metastasizing Ameloblastoma. Path Res Pract 1985. [Google Scholar]
- R A Zwahlen, K W Grätz. Maxillary ameloblastomas: a review of the literature and of a 15-year database. J Craniomaxillofac Surg 2002. [Google Scholar]
- D Campbell, R.R Jeffrey, F Wallis, G Hulks, K.M Kerr. Metastatic pulmonary ameloblastoma. Br J Oral Maxillofac Surg 2003. [Google Scholar]
How to Cite This Article
Vancouver
Kadapathri A, Munnangi A, Pillai V, Vidya V, Shetty V. Ameloblastic carcinoma: A case series, including a case with pulmonary metastasectomy [Internet]. IP Indian J Anat Surg Head Neck Brain. 2025 [cited 2025 Sep 07];6(3):108-112. Available from: https://doi.org/10.18231/j.ijashnb.2020.028
APA
Kadapathri, A., Munnangi, A., Pillai, V., Vidya, V., Shetty, V. (2025). Ameloblastic carcinoma: A case series, including a case with pulmonary metastasectomy. IP Indian J Anat Surg Head Neck Brain, 6(3), 108-112. https://doi.org/10.18231/j.ijashnb.2020.028
MLA
Kadapathri, Abhimanyu, Munnangi, Ashwini, Pillai, Vijay, Vidya, Vidya, Shetty, Vivek. "Ameloblastic carcinoma: A case series, including a case with pulmonary metastasectomy." IP Indian J Anat Surg Head Neck Brain, vol. 6, no. 3, 2025, pp. 108-112. https://doi.org/10.18231/j.ijashnb.2020.028
Chicago
Kadapathri, A., Munnangi, A., Pillai, V., Vidya, V., Shetty, V.. "Ameloblastic carcinoma: A case series, including a case with pulmonary metastasectomy." IP Indian J Anat Surg Head Neck Brain 6, no. 3 (2025): 108-112. https://doi.org/10.18231/j.ijashnb.2020.028
