- Visibility 188 Views
- Downloads 20 Downloads
- DOI 10.18231/j.ijashnb.2020.033
-
CrossMark
- Citation
Primary tuberculous myositis of sternocleidomastoid and anterior scalene muscle: A report of three cases
- Author Details:
-
Madhu Priya
-
Sumeet Angral
-
Rachit Sood
-
Manu Malhotra *
-
Abhishek Bhardwaj
-
Manish Kumar Gupta
Introduction
Mycobacterium tuberculosis, an aerobic bacillus, discovered by Robert Koch in 1882, is the causative organism of one of the most devastating diseases in the world i.e. tuberculosis. It causes chronic inflammation and progresses to form granulomas, leading to necrosis and fibrosis with or without calcifications. According to World Health Organization (WHO), the incidence of tuberculosis was estimated to be around 10 million in 2017, 44% of which occurred in the region of South East Asia.[1] The annual incidence of tuberculosis in India is about 1.5%, with lung being the most common site. Extrapulmonary TB is seen in 2.5% of the cases, out of which only 3% cases have musculoskeletal involvement. Petter reported 0.015% incidence for primary muscular tuberculosis.[2] This diagnosis is very frequently missed due to its rarity and non-specific presentation clinically, which results in delayed treatment.
Here, we report one case of primary tubercular myositis in sternocleidomastoid with anterior scalene muscle involvement and two other cases of purely sternocleidomastoid muscle tuberculosis with no underlying bone or lung pathology.
Case 1
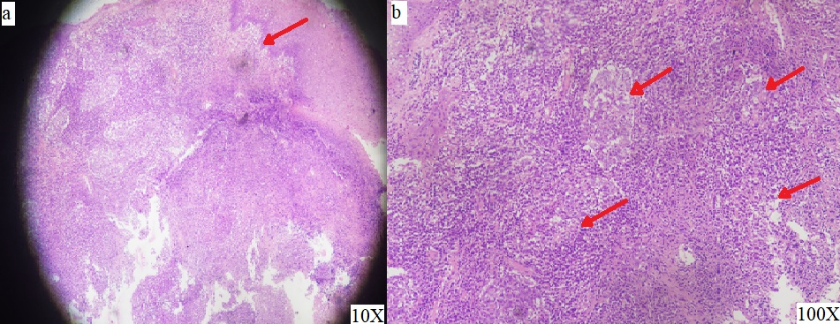
A 43-year-old female presented with chief complaints of gradually progressive anterior neck swelling for 2 months. There was initially no history of pain or pus discharge from the swelling but later progressed to erythematous skin discolouration associated with pain. There were no systemic complaints. She had no past history of pulmonary or extra pulmonary tuberculosis and no contact history. On examination, a solitary 4 x 4 cm soft to firm, tender swelling was present in the anterior aspect of neck just above the supra sternal notch, more towards the right-side clavicle end. Overlying skin discoloration was present with fluctuation in the centre and local rise of temperature ([Figure 1]a). There was no locoregional lymphadenopathy. Her total leukocyte counts were 6790 cells/mm3 with a differential lymphocyte count of 25%. Chest X ray was unremarkable. CECT neck and thorax showed an ill-defined heterogeneously enhancing collection with internal necrotic area at supra and infraclavicular region crossing midline, measuring 4.5x4x2.7cm. The collection was extending into right sternocleidomastoid and right anterior scalene muscle. It was abutting the right lobe and isthmus of thyroid ([Figure 1] b,c,d)). Fine needle aspirate from the swelling showed ill-defined granulomas along with lymphocytes and necrosis in a haemorrhagic background, suggestive of necrotising granulomatous inflammation ([Figure 2] a,b). Ziehl Neelson stain was negative for acid fast bacilli. The swelling ruptured spontaneously at the site of FNAC and tissue with pus, underwent histopathological examination and Gene Expert. Gene Expert was positive for Mycobacterium tuberculosis Culture and KOH stains were negative.
The patient was then started on anti-tuberculosis therapy and improved symptomatically.
Case 2
A 30-year female presented with discharging sinus along lower end of right sternocleidomastoid muscle ([Figure 3] a,b). Cervical sinus was thought of as a possibility. However, pus sent for CBNAAT examination was positive for tuberculosis. Patient’s CXR was unremarkable ([Figure 3]c). No history of contact with T.B. was identified. USG neck revealed collection in infraclavicular end of sternocleidomastoid muscle with a discharging sinus. There was no locoregional lymphadenopathy. Patient was started on anti-tuberculous drugs and responded well.
Case 3
A 25-year-old patient presented with fluctuant swelling in anterior part of neck more towards right just above the suprasternal notch. Skin overlying the swelling was erythematous ([Figure 4]a). CT neck revealed heterogeneously enhancing collection/lesion approx. 49mm x 34mm in midline in infrahyoid, pretracheal and presternal region. The lesion was seen involving the infraclavicular end of right sternocleidomastoid and reported to be of infective aetiology with mild subcutaneous fat stranding ([Figure 4]b). A necrotic lymph node was seen on left side. FNAC from fluctuant area revealed granulomatous inflammation ([Figure 4]c) and CBNAAT was positive for tuberculosis. There was no evidence of pulmonary tuberculosis. Patient responded well with antitubercular drugs.



Discussion
Heffner in 1977 first described focal myositis as a local, self-limiting inflammatory lesion in skeletal muscle having unknown etiology. [3] It usually presents as painful swelling overlying a skeletal muscle with either minimum or no systemic features. There is typically no history of trauma. [4] As skeletal muscle is not a favourable site for growth and survival of mycobacterium tuberculosis, tuberculosis in soft tissue without an underlying pathology is very rare. This is due to high lactate content, poor oxygen, rich vascular supply, highly differentiated state of muscle tissue and absence of lymphatic system. [5] Tuberculosis can spread directly to the skeletal muscles from bone through synovium of tendon sheaths, joints or by direct inoculation or rarely hematogenously.
The diagnosis is often missed due to lack of typical signs and symptoms and rare incidence. The delay in diagnosis and treatment leads to wider spread, deformity and atrophy of the involved muscles. In our cases, tuberculous involvement in sternocleidomastoid and anterior scalene muscle seems primary because there were no tuberculous foci in any other part of the body.
Although culture and histopathological examination is the gold standard for diagnosis, GeneXpert (Semi Nested Real Time PCR) can be used as an effective tool for rapid diagnosis. A negative ZN stain for AFB, normal chest radiograph, with no contact history of tuberculosis and no active tubercular foci does not rule out the diagnosis of tuberculosis. A high index of suspicion is required in a TB endemic country like India, for early diagnosis and treatment.
Cervical tubercular lymphadenitis is known as scrofula. Lymphadenitis is the Most common form of extrapulmonary tuberculosis is lymphadenitis that can be inguinal, cervical, mediastinal, axillary or mesenteric. In immunocompetent and HIV-negative individual lymphadenitis is usually localised unilaterally and in cervical region. In HIV-positive or immunocompromised, it is mostly multifocal and associated with systemic features like weight loss and fever. Lymph nodes initially are nontender, discrete and firm, later becomes a firm matted mass, and finally becomes fluctuant that spontaneously drain and form sinus. Other mycobacteria that may be responsible are M. avium intracellulare complex and M. scrofulaceum.
Commonest sites for extrapulmonary disease are: cervical (scrofula) lymph nodes retroperitoneal and mediastinal. Neck along the sternocleidomastoid is the most common site for tuberculous lymphadenitis (scrofula) that is usually unilateral and causes only little pain. Advanced tuberculous lymphadenitis may suppurate to form a draining sinus. Pathologically these lesions are similar to pulmonary tuberculosis.
Regions affected by TB in the head and neck are oral cavity, pharynx, larynx, middle ear and lymph nodes. Because of its different sites of involvement and varied presentation, TB in head and neck region is interesting from research point of view. These lesions often mimic malignancy and are misdiagnosed, resulting in unnecessary delayed diagnosis. Tuberculosis is extremely rare in skeletal muscles.
Primary tuberculous myositis in skeletal muscle with no underlying pathology has been rarely reported in medical literature. Most of the literature is that of early 20th century. There have been few reported cases of musculoskeletal tuberculosis in sternocleidomastoid muscle, triceps muscle and in the thigh. However, TB can manifest in various forms and can involve any organ.
Muscular TB is a rare localization of the disease (0.01 to 2%).[6] It rarely occurs without bony involvement. Muscular TB is often misdiagnosed as muscular tumor, MRI is useful in such scenario because it specifies the extent of the muscular lesions and helps to orient the site for muscular biopsy. The diagnosis is essentially based on histology.[6] However, in our case CT neck sufficed the extent of lesion.
Here we have reported the series of three cases who presented with anterior neck swelling (in case 1 & 3) and discharging sinus (case 2) wherein diagnosis of isolated tuberculosis of sternocleidomastoid muscle was done incidentally on histopathological examination and confirmed on CBNAAT. In these cases, differential diagnosis of clinical suspicion of soft tissue neoplasm or muscular tumor or branchial sinus initially comes to mind.
Pulmonary tuberculosis can be associated with rare locations such as tenosynovial or bursit tuberculosis, but in both cases, mycobacterium tuberculosis was unusually isolated.[7], [8] In muscular form, the muscle is most often contaminated by a direct neighbouring joint extension or rarely by haematogenous spread as earlier mentioned.[9] Clinical presentation may be only limited to that of neck swelling or discharging sinus with no constitutional symptoms as was seen in all our three cases. There may be associated pain.
The combination of clinical tests with radiological and cytopathological imagery provide strong clues pointing to a diagnosis of skeletal muscle tuberculosis. High suspicion is needed to diagnose at the earliest and to prevent complications especially in endemic areas.[10], [11]
Treatment is based on antitubercular therapy (susceptible to organism) with a minimum of four drugs for a prolonged period. Isoniazid, rifampicin, pyrazinamide and ethambutol regimen is used. Surgical intervention can be an adjunct to antitubercular therapy.[12] The optimum duration of treatment is always debated; treatment should be prolonged to minimum nine months because the short antitubercular therapy may not be appropriate for extrapulmonary TB specifically for osseous inolvements.[12]
Conclusion
Primary tuberculous myositis is a rare but aggressive extra pulmonary manifestation of tuberculosis. Early diagnosis and high index of suspicion remains the mainstay. Gene -expert in today’s era proves to be gold standard. Anti-tubercular therapy should be given as early as diagnosis is established to avoid atrophy and deformity of the involved muscle. This entity should also be included as an important differential diagnosis of neck swellings.
Conflicts of Interest
All contributing authors declare no conflicts of interest.
Source of Funding
None.
References
- . World Health organisation. Global tuberculosis report. 2019. [Google Scholar]
- S A Kulkarni, P Kulkarni, U S Udgaonkar, S A Gadgil. Primary Tuberculous Myositis: A Rare clinical entity. Indian J Tuberc 2013. [Google Scholar]
- RR Heffner, VW Armbrustmacher, KM Earle. Focal myositis. Cancer 1977. [Google Scholar] [Crossref]
- C Georgalas, L Kapoor, H Chau, A Bhattacharyya. Inflammatory focal myositis of the sternomastoid muscle: is there an absolute indication for biopsy? A case report and review of the literature. Eur Arch Oto-Rhino-Laryngol 2006. [Google Scholar] [Crossref]
- C K Petter. Some thoughts on tuberculosis of fascia and muscle. Lancet 1937. [Google Scholar]
- S Rehm-Graves, AJ Weinstein, LH Calabrese, SA Cook, FRS Boumphrey. Tuberculosis of the greater trochanteric bursa. Arthritis Rheumatism 1983. [Google Scholar] [Crossref]
- I. F. Abdelwahab, S Kenan, G Hermann, M J Klein. Tuberculous gluteal abscess without bone involvement. Skeletal Radiol 1998. [Google Scholar] [Crossref]
- M Chapman, R O Murray, DJ Stoker. Tuberculosis of the bones and joints. Semin Roentgenol 1979. [Google Scholar] [Crossref]
- W W Plummer, S Sanes, W S Smith. Muscle Tuberculosis. J Bone Joint Surg 1934. [Google Scholar]
- J Y Wang, L N Lee, P R Hsueh. Tuberculous myositis: a rare but existing clinical entity. Rheumatol 2003. [Google Scholar]
- E Serhan. A visible and palpable cause of backache. Ann Rheumatic Dis 2000. [Google Scholar] [Crossref]
- . Treatment of tuberculosis-Guidelines for national programmes. 3rd Edn. 2003. [Google Scholar]
