Introduction
Pulp necrosis followed by trauma or dental caries if left untreated may lead to periapical pathologies like peri apical granuloma & cystic lesions. Periapical surgery is indicated in cases where conventional root canal therapy fails.1 The main cause of unsuccessful endodontic therapy is presence of infected tissue in endodontic spaces.2 Periapical surgery is aimed to remove periapical pathology followed by complete soft tissue & radiographic bone healing. Successful endodontic therapy depends on complete periapical repair & regeneration of soft tissue & bone.3, 4 The teeth undergoing apical surgery have less predictable prognosis, so the possibility of accelerating bone regeneration in surgical defects in periapical region is important, as even a single tooth can be strategic in prosthetic rehabilitation. Bone & soft tissue regeneration can be achieved by local application of hormones, growth factors & plasma derivatives as advocated by studies.5 Bone morphogenic proteins, parathyroid hormone, platelet-derived growth factor, platelet rich plasma, & enamel matrix proteins have been applied to promote healing of surgical wounds /defects.6, 7, 8, 9
Platelet rich fibrin a biologic revolution constituted by fibrin network of platelets, leukocytes, cytokines, stem cells, & three dimensional architectures, which favours wound healing & immunity.10 Platelets in PRF are capable of releasing platelet derived growth factor (PDGF) transforming growth factor β1 (TGF β1), insulin like growth factor (IGF) & exhibit varied potent local properties like cell migration, cell attachment, cell proliferation & cell differentiation even up to one week.11, 12
Materials and Methods
This prospective randomised, controlled clinical Study was performed in the department of OMFS. Study was conducted on 40 patients diagnosed with periapical lesions in maxilla. Patients were divided into two groups, Group A & B comprising of 20 patients each. Diagnosis was made on History, clinical & radiographic examination of patient.
Operative procedure
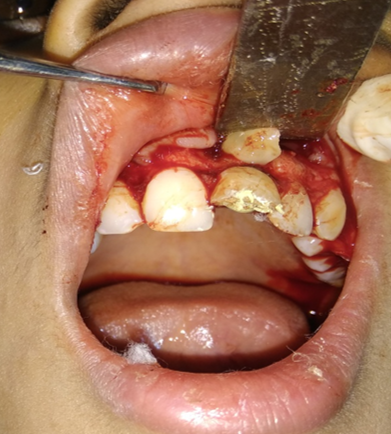
A Standard periapical surgery procedure was performed. After removal of periapical pathology by enucleation, curettage & Apicoectomy PRF clot was inserted in surgical cavity in Group A. Whereas in controlled group (Group B) surgical cavities were left empty. Flap closure was done using 3.0 black silk. Sutures were removed on seventh post-operative day. Post-operative analgesics, antibiotics & instructions were given to all patients
Preparation of PRF gel
PRF gel was prepared by protocol given by Choukroun et al 13
1.5 ml of venous blood was drawn in a tube without anticoagulant & was immediately centrifuged at 3000rpm for 10 minutes .Blood clot was extracted using sterile forceps & separated into 3 layers.
Upper straw-coloured layer acellular plasma was removed.
The middle layer containing PRF was collected 2mm below the lower diving line.
Third red coloured layer, lower fraction containing red blood cells.
Follow up of the patient was done on 3rd, 5th & 7th day post operatively. Radiographic evaluation of bone regeneration was done in three, Six, nine & 12 months. No of analgesics consumed from first day to 7th day, swelling, healing of wound, any other complication was recorded during follow-up. Patients were given questionnaire & instructed to record their pain level using Visual Analogue Scale (VAS). Soft tissue healing was assessed by healing index reported by Landry et al.14 which depends on tissue colour, presence of bleeding on palpation, epithelialization of wound margin granulation tissue & suppuration.
Results
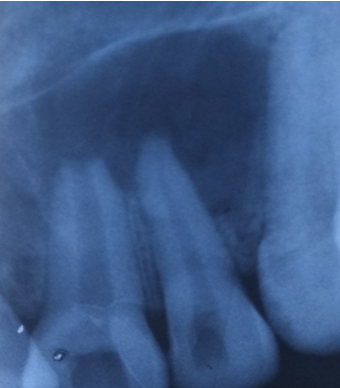
In this study in PRF group pain was reported significantly less & patients consumed less analgesics compared to control group from third post-operative day on wards. Post-operative intra & Extra oral swelling was evaluated after 24, 48, 72 hours & 7th post op day. No difference was seen in swelling & soft tissue healing in both groups. At 3 months, PRF group exhibited better bone healing than control group. Bone density was assessed by comparing bone formation in both groups (PRF & Non PRF) using intra oral periapical radiographs & Orthopantomographs at first, 3rd third 6th , 9th & 12th months post operatively. Highly Significant bone formation was noted in PRF group at 3rd month & bone healing was almost complete on 6th month. Non-PRF group (Control) showed slow radiographic bone healing. Bone healing was complete between 9-12 months.
Discussion
Choukroun et al13 in France first discovered platelet rich fibrin (PRF) an autologous fibrin matrix to enhance bone regeneration. PRF is easy, simple inexpensive process & requires no additive in comparison to platelet rich plasma (PRP). PRP requires artificial biochemical adding for modification & neutralising the anticoagulant. The addition of bovine derived thrombin to promote conversion of fibrinogen into fibrin is also eliminated.15 PRF is a by -product of patients own blood therefore chances of transmission of infectious disease is rare & patients need not to bear the expense of harvesting procedure in hospital.16
The result of present study shows that PRF is efficient in decreasing pain & less consumption of analgesics by study group as compared to controlled group. This study is in accordance with the studies carried out by Kumar et al17 & Ahmed et al18 who also revealed that PRF significantly reduced post-operative pain & less analgesic consumption after third molar surgery.
In the present study intra, oral swelling was evaluated & classified as Mild, Moderate & sever according to clinical visual evaluation. Extra oral swelling was evaluated by tape measurement in horizontal direction from midline to last point of swelling. Measurement in vertical direction was done from supraorbital margins to maxillary occlusal plane. This study didn’t show any significant difference in post operatively intra & extra oral swelling between controlled & study group similar to the studies reported by Uyanik et al. 19
Jeyaraj et al20 & Marenzi et al21 demonstrated better soft tissue healing clinically on 3,7, &14 days after surgery in study group in extraction sockets than controlled group. Contrary to this, present study did not show any difference in soft tissue healing in both groups.
The studies by Hauser & Gaydaro22 demonstrated that there is increase in bone density from third to sixth month. Their analysis showed significantly improved architecture & higher bone quality in PRF Group .Similarly radiographic studies done by Alzahrani et al23 showed significant difference in bone formation in study group at one, four & eight weeks. Choukroun & Diss indicated that when PRF membrane is used new blood vessels are generated & epithelialization is promoted which facilitates rapid wound coverage. The present study also showed marked bone healing of surgical cavity from 3rd month & at 6th month radiographic bone healing was complete in PRF group. In Non PRF group radiographic bone, healing of surgical cavities was complete between 9-12 months.
Simonpieri et al24 reported that the use of platelet & immune concentrate offers following advantages 1) Fibrin clot plays important role & serves as biologic connectors between bone particles. 2) integration of this fibrin network into regenerative site facilitates cellular migration, particularly for endothelial cells necessary for neoangiogenesis & vascularization. 3) the platelet cytokines (PDGF, TGF-a, IGF-1) are released gradually as the fibrin matrix is resorbed thus creating a perpetual process of healing. 4) The presence of leukocytes & cytokines in the fibrin network also plays a significant role in self-regulation of inflammatory phenomenon within grafted material
Conclusion
The present study concluded that PRF is a part of new biotechnology & a healing biomaterial as it contains all the factors required for better & optimal consolidation of bone formation. The application of PRF gel made of intact platelets & fibrin by high-speed centrifuge provides an ideal scaffold for bony tissue repair in periapical surgeries. PRF placement showed promising result in stimulating bone formation after 3 months of surgery & reduced post-operative discomfort. However, Long-term follow up may be required to evaluate the final treatment outcome.