Introduction
Spinal epidermoid cysts are rare benign tumors comprising 1% of the all spinal tumors.1 They comprise between 0.5% and 1% of all spinal tumors but account for up to 10% of intraspinal tumors in children.2 First case of spinal epidermoid cyst was reported by Chiari in 1883.3 Penisson-Besnier et al. firstly reported an intramedullary EC diagnosed by MRI(3). Octavian M S et al reported a total of 139 cases of spinal epidermoid cysts dated from 1962 to 2019 with their case included. 4 They reported a bimodal age distribution with females affected more than males. Beechar V et al reported a case of spinal epidermoid cyst in a 71 year old hypertensive female extending fromT 10- S1.5 This brings the total number of spinal epidermoid cysts to 141, including our case.
A literature review by Barbagallo GMV et al revealed that only eight cases of isolated spinal intraduralextramedullary epidermoid cysts had been reported, six cases of which were in the thoracic region.6 Akgun B et al. reported A case of intraduralextramedullary epidermoid cyst in a 3-year-old male at L1-L2 level presenting with increasingly leg weakness.7 Ganapathy S et al. reported another case of spinal intraduralextramedullary epidermoid cyst in a 1-year old female child at the level of D-10, presenting to the outpatient clinic with a brownish discoloured skin patch on the back with a slight swelling observed since birth.8 This brings the total number of reported spinal intraduralextramedullary epidermoid cysts to 11, including ours out of which only 8 are reported in thoracic location.
Thoracic region is the commonest site of spinal epidermoidcyts, followed by the lumbar region and least commonly, the sacral and cervical regions.9 The presentation could be asymptomatic with incidental findings or could present with motor, bowel and bladder, sensory or pain disturbances based upon the location of the cyst. The most frequent symptom reported was pain, followed by motor deficit, sensitive deficits, and sphincter deficiencies. 4
Histologically these cyts are lined by stratified squamous epithelium and due to continuous desquamation and keratine breakdown, characterstic contents of the cyst are formed. They cysts are classified as congenital when associated spinal dysraphism, 10 or acquired due to repeated lumbar puncture and trauma. Congenital spinal epidermoid cysts unassociated with spinal dysraphismare very rare. 1, 8, 9 Here we are presenting arare and interestingcase of isolated spinal epidermoid cystthat presented as intradural and extramedullary in thoracic location D1 with review of the relevant literature.
Case Summary
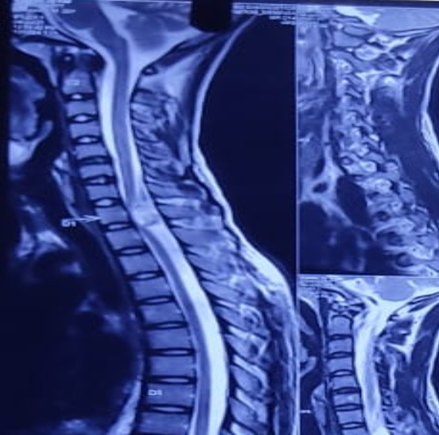
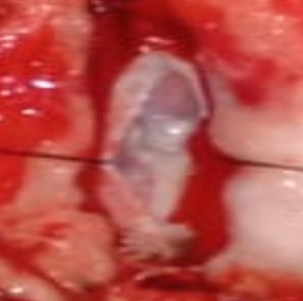
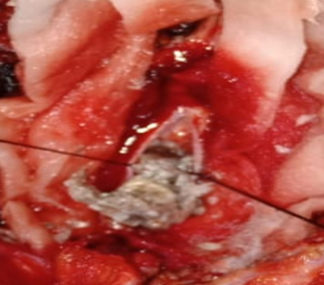
A 22 year male presented in casualty with complaints of pain in both lower limb and difficulty in walking since 2 months with no co-morbidities. On neurological examination, spastic weakness was present in both lower limb with no involvement of the bowel and bladder. No features suggestive of spinal dysraphismwere observed. There was no evidence of spinal dysraphism, the congenital nature of the lesion could not be established. Also, there was no hisFigure 3 tory of trauma and lumbar puncture. As such, the case was considered as an isolated case of spinal intradural epidermoid cyst. Contrast enhanced Magnetic resonance Imaging (MRI) of spine revealed an intradural extra medullary well defined cystic lesion at D1 level, partially compressing the spinal cord. The lesion wasisointense on T1 weighted image and non-homogenous to hyperintense on T2 weighted image with no significant contrast enhancement (Figure 1). There was no radiological evidence of osseous changes such as expanded spinal canal, laminar thinning and vertebral body scalloping. On surgical intervention intraduralextramedullary epidermoid cyst was found and total excision was achieved (Figure 2). Decompression of the cyst revealed cheesy material corresponding to keratin (Figure 3).
Histological examination of the specimen with extensive sampling revealed afibrocollagenous cyst wall lined with keratinizing stratified squamous epithelium with preserved granular layer. No adnexal structures such as eccrine glands, sebaceous glands or hair follicles were seen in the wall. Cyst contents were composed of abundant keratin flakes. Post operative period was uneventful with a progressive recovery and patient was discharged on post operative day 14 and is asymptomatic on follow up.
Discussion
Spinal epidermoid cysts are rare benign tumor and comprise 1% of all spinal tumors.1, 2 On review of literature only few case reports are stratified for spinal epidermoid cyst without other spinal dysraphism, trauma and lumbar puncture.1, 2, 3 Review of literature in the present study revealed, that the age ranged between 1 to 71 years.
In their review Octavian M S et al.4 reported that congenital cysts were 62.9% while acquired cysts are seen in 38.1% of patients. Congenital epidermoid cysts are usually associated with spina bifida, dermal sinus tract and other neural tube defects such asmyelomeningocele, spina bifida occulta, spinal cord lipoma, scoliosis cutaneous/dermal defects.9, 10 The possible explaination for congenital epidermoid cysts are the abnormal inclusion of ectoderm tissue in the neural tube during its closure in the intrauterine life. The most common localization was in the lumbar area and one third of the tumors were intramedullary.4 Acquired epidermoid cysts have been mostly reported in the region of the cauda equina (below the L1 level),10 because lumbar punctures are usually performed around the level of the iliac crests.
Histopathologicallyepidermoid cyst is lined by stratified squamous epithelium and cyst contents are formed due to progressive desquamation and keratin breakdown. The feature that differentiates it from dermoid cysts is the absence of skin appendages on histological examination (sebaceous glands, hair follicles, sweat glands)
Spinal ECs are difficult to diagnose on clinical symptoms alone. Plain X-rays usually show normal or nonspecific findings. Contrast MRI modality is the investigation of choice in these cases. These tumors are well defined, isointense on T1 weighted image, hyper intense on T2 weighted images with no or minimal contrast enhancement and the cyst content has signal similar to CSF.11, 12 Generally, there is no perilesional edema. Presence of the typical signal intensity elicited on MRI helped to gird the diagnosis.
Intraoperatively, as white masses that are encapsulated and are commonly referred to as “pearly tumors.”.5 Complete resection of the encapsulated tumor is difficult for all cases, because the cyst wall is very thin and often adhered to the arachnoid membrane, spinal cord, or nerve roots. adherence to surrounding tissues is remnant, it may lead to recurrence of the cyst Thereby, subtotal resection is also commonly performed.10, 13, 14 However total excision of epidermoid cyst is the main goal of surgery.15 There is high chance of neuronal damage during removal of cyst wall because sometimes cyst wall densely adheres with spinal cord and arachnoid membrane. Moreover, avoidance of cyst content spillage into subarachnoid space is critical to prevent the development of chemical meningitis and arachnoidal adhesions that may develop postoperatively.16 Octavian M S et al.4 in their literature review reported a good surgical outcome in most of the treated cases. In our case, we achieved total excision of epidermoid cyst owing to the non adherent cyst walls, with almost no damage to the surrounding neuronal tissues and structures.
Conclusion
Thoracic intraduralextramedullary epidermoid cysts are rare benign, slow growing tumors which should be considered in the clinical differential diagnosis in this location. A possibility of the occurrence of sporadic cases despite the absence of a history of spinal dysraphism and puncture, such as in our case, should be considered. Total excision without neuronal damage is the main goal of surgery. Hence, safe maximum excision should be primarily aimed for and is considered the ultimate curative treatment, along with a long-term follow up to rule out any possible risk of recurrence.