Introduction
Post-traumatic CSF leaks occurs in 1% to 3% of all closed traumatic brain injuries (TBI) in adults. In adults, 80% to 90% of CSF leaks result from head injuries. 1, 2 Traumatic CSF leak is reported in 10% to 30% of the skull base fractures in adults.2 Anterior skull base fractures are five to six times more common than middle and posterior skull base fractures amongst all cases of skull bases fractures. 3, 4 Dural tears are common because of the firm adherence between the duramater and the skull base. 5, 6, 7 CSF rhinorrhea may be accompanied with other symptoms, including clear nasal discharge and headache. Patients may further develop complicationssuch as pneumocephalus, meningitis, or brain abscess. 8 Post traumatic CSF leak can be potentially dangerous when it gets complicated with bacterial meningitis if not self-resolved. 9, 10 Meningitis is known to occur in 20 to 56% of patients and mortality may be as high as 10%. 11, 12, 13, 14 In few cases CSF Rhinorrhea and pneumocephalusmay occur years after ACF Base fracture.This could be due to fresh trauma causing scar dehiscence. 15, 16, 17, 18 Early detection and immediate measures to stop CSF rhinorrhea plays an important role in preventing complications and improving outcomes. More than half of these CSF leak is presented within 48 hours of the trauma while almost all CSF leaks occur within 3 months in delayed manner. 19 The most common fracture sites leading to CSF leaks following TBI are the frontal sinus (30.8%), sphenoid sinus (11.4–30.8%), ethmoid (15.4–19.1%), cribriform plate (7.7%), fronto-ethmoid (7.7%) and sphenoethmoid (7.7%).20, 9
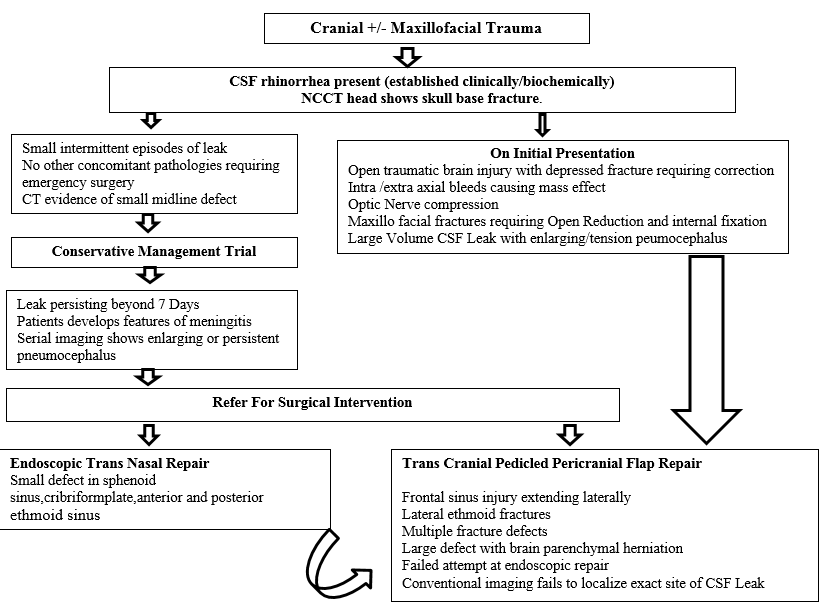
With the advent of endoscopy more and more cases are being successfully treated by endoscopic repair. Still there is a subset of patients who require and benefit from Trans cranial repair. This study attempts to classify patients with CSF rhinorrhea into three groups based on clinico- radiological findings and further proposes a management algorithm for definitive management.
Materials and Methods
This was a retrospective study carried from 2014 to 2020 in which all patients of traumatic CSF rhinorrhea reporting to tertiary care service hospital were included. Based on the clinico-radiological profile they were placed in three broad groups. Group A consisted of patients who were given a trial of conservative management. In case CSF rhinorrhea persisted beyond 7 days they were offered definitive surgery. Group B consisted of patients who were managed with Tran’s nasal endoscopic repair. Group C consisted of patients who were treated with Trans cranial pedicledpericranialrepair. The mechanism of injury, site of ACF base fracture, other associated lesions and complications following treatment by all three modalities of treatment were analyzed and conclusions drawn. Based on the results from this study an algorithm has been drawn for management of Post traumatic CSF rhinorrhea.
Conservative management
The following guidelines were followed-
Bed Rest, Head elevation avoidance of straining, coughing sneezing with symptomatic therapy including laxatives, cough suppressants Etc.
CSF culture to be sent at time of presentation and Parenteral antibiotics started. In case of positive culture report; parenteral antibiotics should be continued for 2 weeks.
Lumbar Drain may be considered when leak persists
Conservative management was carried for 4 to 7 days. However, cases with large defects, other associated pathologies and enlarging pneumocephaluswere offered early surgery.
Indications for surgery
Extensive bone defects in the cranial base, multiple fractures of the ethmoid bone and the posterior wall of the frontal sinus.
Leak is associated with concomitant pathologies requiring surgery. Concomitant treatments included elevation of depressed cranial vault fractures, repair of direct open head injury,and removal of space-occupying hematomas, facial fracture reduction & stabilization, external CSF drainage, decompression of the optic nerve, post-traumatic intracranial infection.
CSF leak is severe, recurrent, or not amenable to the endoscopic treatment
Persistent CSF Rhinorrhea which is not localizable by conventional imaging
Surgical technique of trans cranial pedicle peri cranial repair
Position: Head is placed in neutral position over silicone ring. This helps in easy maneuverability during bifrontal craniotomy and subsequently also permits sufficient extension during skull base repair.
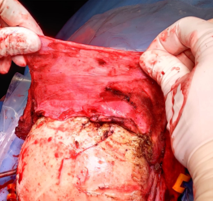
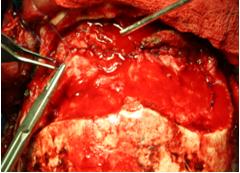
While raising the bicoronal skin flap the pericranium is left intact. Following reflection of scalp flap,pericranial flap can be lifted more proximal from the incision site thereby providing a wide tension free pedicled flap for covering the ACF base.[Operative Figure 3, Figure 4].
Attempt to raise a single bone flap by carefully separating the midline superior sagittal sinus using sharp periosteal elevator.
Following durotomy ligate the sagittal sinus close to skull base [Operative Figure 5]
Avoid damage to bridging veins as much as possible,especially if they are large and dilated.
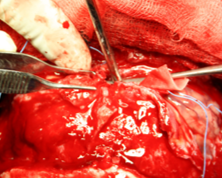
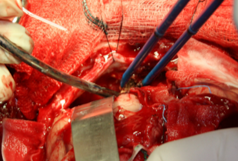
While retracting the brain move from lateral to medial part of ACF Base use a narrow brain spatula and decompress the cisterns in early part of surgery. Also avoid fixed brain retraction. These two maneuvers will reduce the incidence of lobar retraction injury.[Operative Figure 6].
The site of CSF fistula is identified keeping in view the imaging findings.The hall mark would be to find adherent arachnoid and brain parenchymal herniation into the defect.
For midline defect the olfactory nerve is sacrificed. This helps in lifting the bifrontal lobe away from the ACF Base thereby permitting full inspection and easy repair.
Flow able hemostats are a useful adjunct to occlude the defects prior to proceeding with repair.
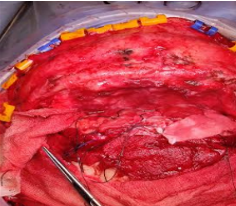
While placing the carpet of pedicledpericranial flap ensure that it rolls over the ACF base margins loosely and adheres firmly to the entire ACF base.[Operative Figure 7].
Tacking sutures along the sphenoid ridge margins and on planumsphenoidale help in preventing slippage of graft.
Ensure loose but watertight duroplasty after repositioning the frontal lobe. The tamponed effect due to frontal lobe ensures firm adherence of pericranial graft over the ACF Base.[Operative Figure 8].
Any skull base defect more than 5 square mm in area will preferably require bone graft reinforcement before doing carpet repair.
Following dural closure a valsalva maneuver will help in confirming the watertight closure.
Cranialization of frontal sinus if exposed must be performed meticulously.Frontal bone flap is then repositioned and fixed. [Operative Figure 9].
During anatomical closure a subgaleal drain with moderate suction pressure ensures early wound healing.
Observation
A total of 54 cases were included in this study.30 cases were given a trial of conservative management. Of these 06 had persistent CSF rhinorrhea beyond 7days. They were thereby transferred to Group B and C (4 of those to endoscopy group i.e. Group B and 2 to Trans cranial group i.e. Group C). Hence, 24 were managed conservatively, 10 by Endoscopic repair and 20 by transcranial repair).
Evaluation of trauma mechanism showed that two-wheeler road traffic accidents was the commonest cause of trauma leading to CSF rhinorrhea (Table 1). A study of site of trauma at ACF Base revealed that cribriform plate was the commonest site of fracture and CSF rhinorrhea (Table 2). The complications of each modality of management (Table 3) showed that endoscopically managed cases had no failures. Of total 54 cases, 8 required early surgery based on clinico-radiological presentation. (Table 4).
The Trans cranial repair although more demanding was easy to master. With each successive procedure the complications and recovery rates reduced thereby improving outcomes.In comparison with other management modalities it had certain distinct advantages and disadvantages.
Result
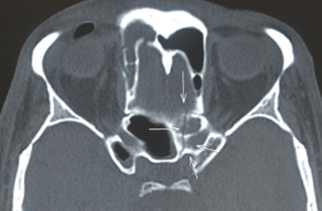
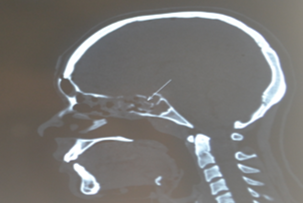
Our study shows that based on the presentation and radiological findings post traumatic CSF rhinorrhea can be managed conservatively, or by definitive surgery. Majority of the case respond well to conservative management (Figure 2) although endoscopic repair offers lesser morbidity its applicability is only for a select group of patients having small midline defects. Pedicle pericranialtranscranial repair is a procedure which can be performed in a patient group with definite indication. The outcomes are reasonable and the morbidity is acceptable considering the fact that it results in prevention of meningitis and other serious infections of Central Nervous system. In our study except for one case which required confirmation with beta 2 transferrin, rest all were diagnosed radio logically and with CSF glucose estimation.Based on location of ACF base defect Trans cranial surgery was offered in all cases as shown in Radiographic picture [Radiograph Figure 10, Figure 11, Figure 12, Figure 13] Based on our experiencewe have proposed a management algorithm for management of Traumatic CSF Rhinorrhea.(Figure 1)
Table 1
Mechanism of trauma leading to anterior skull base fracture with CSF Rhinorrhea
|
Trauma Mechanism |
Numbers |
|
Road Traffic Accident (Two wheeler) |
43 |
|
Fall from height |
06 |
|
Assault |
02 |
|
Other |
03 |
Table 2
Location of Anterior skull base fractures
|
Fracture and defect site |
Numbers |
|
Frontal Sinus |
04 |
|
Cribriform Plate |
08 |
|
Ethmoid |
02 |
|
Sphenoid |
02 |
|
Planum sphenoid |
01 |
|
Mltiple site fractures |
04 |
Table 3
omplications following management of CSF Rhinorrhea in all three groups
Table 4
Clinical presentation of cases subjected to early surgery (total 08)
Figure 2
Showing the distribution of 54 cases managed conservatively, Endoscopically and by Trancranial surgery
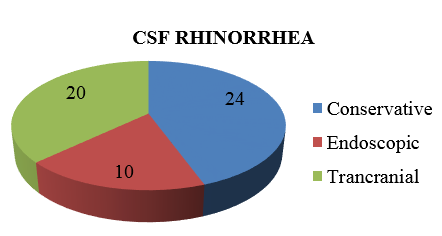
Figure 3
Operative Harvesting of Pericranial Flap being done proximal to scalp incision so as to get enough Flap area for ACF base repair.
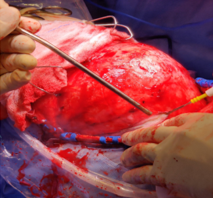
Figure 6
Operative Dynamic frontal lobar retraction to inspect the defect and minimize lobar retraction injury.
Discussion
British neurosurgeon Hugh Cairns, first introduced a classification scheme for CSF rhinorrhea in 1937. He differentiated between spontaneous and postoperative CSF leak.19 In 1926, Dandy was the first to successfully repair a CSF fistula using a tensor fascia lata graft through a transcranial, intradural approach. 21 Followings successful repair technique, various techniques for anterior cranial fossa reconstruction after extensive craniotomy for addressing variousconcomitant pathologies, have been described in the literature. These range from no formal reconstruction to elaborate free flaps with microvascular anastomosis. As on date there is nogold standard technique for any given situation.Reconstruction mustbe tailored depending on the anatomical site and extent of dural and cranial defect. In 1981, German otolaryngologist MalteWiganddid pioneering work in the use of intraoperative endoscope for repair of spontaneous CSF rhinorrhea. 22 since then rapid advances in endoscopic techniques have popularized the use of endoscopy for repair of anterior cranial fossa CSF leaks.23, 9
Endoscopic techniques prove advantageous in the repair of small, spontaneous, and localizable CSF fistulas because they are lesser invasive in addition to offering the advantage of reducing blood loss and operative time. 24 In present day, Classic surgical approaches still play a role and, in fact, prove superior in select cases where the dural defect is extensive or the CSF fistula is not localizable. 25 The rationale behind the need for a watertight dural closure is to effectively separate the intradural and extradural compartments to reduce the postoperative morbidity and mortality associated with persistent CSF leak. We think the advantage of our closure technique is that by using generously sized pericranialgraft, itallows the brain to relax in its normal anatomical position while the natural weight of the frontal lobe may further reinforce this layered closure by tamponade. Defect size is not a limiting factor because large vascularized pericranium grafts can be easily harvested and hitched into position. More importantly, this technique does not require a significant learning curve and is easily mastered. Disadvantage of this technique is that anosmia becomes a permanent disability. Also damage to the bridging veins during ligation of superior sagittal sinus may lead toprolonged hospital stay and morbidity. Although an extensive procedure the dividends are rich and outcomes good.