- Visibility 317 Views
- Downloads 22 Downloads
- Permissions
- DOI 10.18231/j.ijashnb.2021.033
-
CrossMark
- Citation
Intracranial pilocytic astrocytoma with spinal drop metastasis: A case review, discussion of its current management and related literature
- Author Details:
-
Shekhar Kumar Keshri *
-
Satyendra Narayan Sinha
Abstract
Pilocytic astrocytoma (PA) is a low grade benign tumor, commonly occurs in Cerebellum (42-60%), Optic & hypothalamic region (9-30%), Brain Stem (9%). They rarely spread. It rarely occurs within the ventricle. In this report, we described our experience with cranial pilocytic astrocytoma in a 14-year-old child, who initially treated with near total decompression of tumor. Four and half years later, recurrence of primary tumor with obstructive hydrocephalus occurred for which he underwent ventriculo-peritoneal shunt followed by re-excision. As further treatment was being evaluated for radiotherapy in view of recurrence at the primary site, he got detected to have significant spinal drop metastasis seen on MRI Spine. Finally, he underwent craniospinal irradiation (CSI).
Introduction
Pilocytic astrocytoma (PA) is a benign brain tumor that occurs mostly in children and young adults. The tumor is typically slow growing and does not spread. Therefore, pilocytic astrocytomas are typically categorized as WHO Grade I. Spinal drop metastasis in pilocytic astrocytoma is a rare event that likely occurs via cerebrospinal fluid (CSF) pathways as a primary mechanism.[1] Here, we present an unusual case report of pilocytic astrocytoma who initially treated with surgery and later he developed recurrence and spinal drop metastasis. In this report, we discuss the case and review of literature with a focus on treatment options and prognosis of such patient.
Case
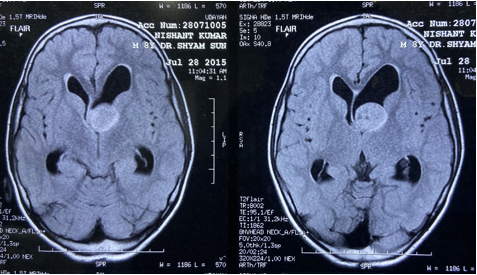
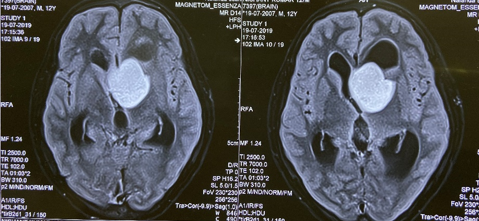
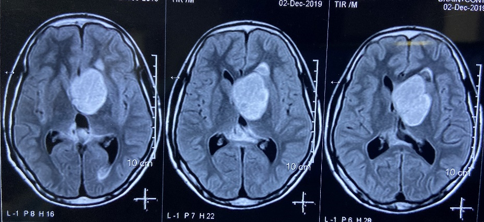
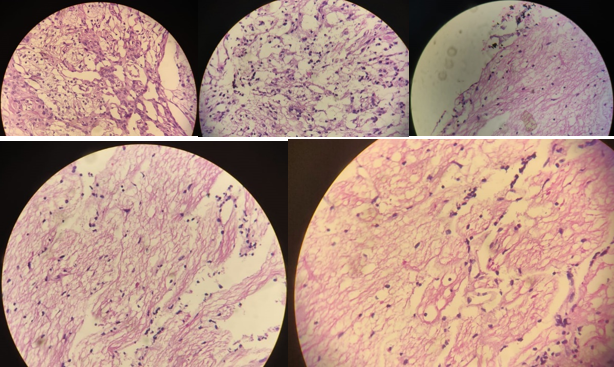
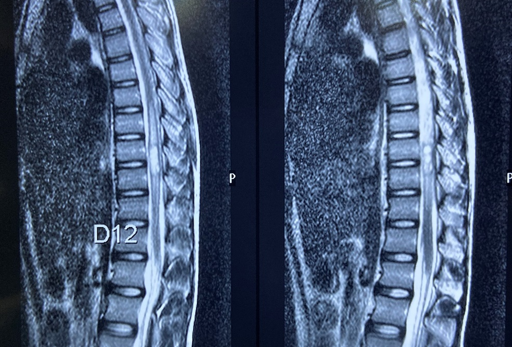
A 14-year-old boy (Age in 2020) was evaluated for severe headache and vomiting for last 6 months in July 2015. MRI brain done in July 2015 showed the presence of 2.2 x 2.1 x 2.0 cm sized lesion involving the left lateral frontal horn near the foramen of monro with small focal nodule seen in continuity with larger lesion along the superolateral aspect ([Figure 1]). He underwent left frontal craniotomy with near total decompression of tumor in August 2015. Histopathology report was suggestive of low-grade astrocytoma – Pilocytic in nature. After four and half years, he started complaining of severe headache and associated with vomiting. MRI Brain was done which showed a 3.5 x 3.0 x 2.8 cm sized centrally enhancing intracerebral SOL in the left anterior periventricular region and medial temporal lobe with compression of anterior third ventricle and left frontal horn with moderate obstructive hydrocephalus ([Figure 2]). In view of obstructive hydrocephalus, Ventriculoperitoneal shunt was placed. Due to some reasons, he defaulted for few months. On follow up again, MRI brain was done in December 2019 which was suggestive of 4.6 x 3.6 x 4.4cm sized well defined lesion seen along left lateral ventricle frontal horn near the foramen of monro ([Figure 3]). This time again he underwent frontal craniotomy and subtotal excision of mass in January 2020. HPE report was suggestive of pilocytic astrocytoma ([Figure 4]). In view of recurrent intracranial lesion, he was referred for adjuvant radiotherapy. Before Radiotherapy planning, MRI spine screening was done which showed intramedullary hyperintense lesion of size 6.6 x 7.4 x 20.9 mm in dorsal cord at D9-D10 level with adjoining edema, extending superiorly up to D7 level and inferiorly up to D11 level, strongly suggestive of spinal drop metastasis ([Figure 5]). Power in both upper and lower extremities, bladder and bowel were intact. In view of significant spinal drop metastasis and recurrent intracranial lesion, he was planned and finally underwent craniospinal irradiation (CSI). CSI showed excellent response. In some patients, where the residual disease present, alkylating agents such as temozolomide can be considered as further as adjuvant treatment with maximum possible benefits.
Discussion
Low grade gliomas are characterized by indolent growth pattern and are divided into pilocytic and non-pilocytic subtypes. Pilocytic astrocytoma, also known as juvenile pilocytic astrocytoma. It corresponds histologically to WHO grade I tumor. The neurological signs and symptoms of the tumor are related to tumor localization and its mass effect. [2], [3]
Pilocytic astrocytoma is more amenable to total resection. Complete resection of tumor is associated with excellent survival, with the majority of more than 90 % get cured. Incomplete resection is also associated with long term survival with 70 – 80% patients who survive more than 10 years. The usual recommendation is for close follow-up following gross or subtotal resection and utilizing radiotherapy for tumors that have recurred more than once, or for those with considerable residual disease in a critical location where even slight progression could result in significant morbidity. [4]
Most studies concluded that the extent of surgical resection of the tumor is the main factor that influence the patient’s outcome such as true recurrence, regrowth, or regression of residual tumors. [5], [6], [7] In our patient, initially near total decompression of the tumor was done. This patient was asymptomatic for nearly four and half years, subsequently he developed severe headache associated with vomiting. MRI Brain showed recurrence of intracranial tumor with obstructive hydrocephalus. Ventriculoperitoneal shunt followed by craniotomy with re-excision of tumor mass was done. Since, Patient had recurrent lesion, he was referred for adjuvant radiotherapy this time. Rather, we would suggest radiotherapy for incompletely resected tumours upfront. As a complete Radiotherapy planning process and keeping in mind that pilocytic astrocytomas near ventricles may spread to neuraxis. So, MRI spine screening was done which showed hyperintense lesion of size 6.6 x 7.4 x 20.9 mm at D9-D10 level with adjoining edema consistent with significant spinal drop metastasis.
Low-grade Gliomas (LGG) can disseminate along the neuraxis, either at diagnosis (2%–5%) or at the time of disease progression (5%–12%). [8], [9] Since the use of MRI has become routine in surveying of patients with brain tumors, a sharp increase in number of cases have been reported.[1] Spread mechanisms are not well understood. Tumors of any grade arising nearby to CSF pathways may disseminate. Tumoral mass located in the floor of the third ventricle may breach the ependyma and invade ventricular cavity, resulting in to ependymal or leptomeningeal seeding.[1] CSF analysis for malignant cells and protein is not routinely performed in patients with LGG because positive results are so infrequent, even in cases of spinal dissemination. [10] So, we have not analysed CSF cytology.
Because of the rarity of dissemination within this benign tumor entity, a standardization of treatment misses. Currently, there is no consensus on first or subsequent types of treatment that should be administered to patients with metastatic LGG. In patient who are detected to have synchronously low-grade glioma with spinal drop metastasis, surgical resection of the intracranial mass and debulking of the spinal lesion may be done. [11] Radiation therapy to all or part of the craniospinal axis or subtotal excision of spinal drops are evaluable option for whom in which disseminated disease was identified after initial diagnosis. [9] In some case series and case report, craniospinal irradiation (CSI) was done for treatment of spinal drop metastasis with good outcome. [12], [13]
However, the outcome of patients with spinal drop metastasis is not well known. Nevertheless, it is likely to be not as good as that of patients with localized recurrence or completely resected primary disease. In other way, it is not as bad as the leptomeningeal spread in high grade gliomas.
Conclusion
Pilocytic astrocytomas are low grade gliomas and spinal drop metastasis are exceedingly rare. Such incidence in low grade glioma is seen so infrequently but there is no standard therapy established. Early radiotherapy can be considered for pilocytic astrocytomas where complete radical surgery could not be possible. As evidences suggest, we would recommend Spinal screening with MRI can be considered in these cases to intervene as earliest. Craniospinal irradiation or excision of spinal drops metastasis (if possible) followed by +/- local radiotherapy may be valuable options.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Source of Funding
None.
References
- Figueiredo EG, Matushita H, Machado AG. Leptomeningeal dissemination of pilocytic astrocytoma at diagnosis in childhood: two cases report. Arq Neuropsiquiatr. 2003;61(3B):842-7. [Google Scholar]
- Collins VP, Jones DH, Giannini C. Pilocytic astrocytoma: Pathology, molecular mechanisms and markers. Acta Neuropathol. 2015;129(6):775-88. [Google Scholar] [Crossref]
- Cyrine S, Sonia Z, Mounir T. Pilocytic astrocytoma: A retrospective study of 32 caes. Clin Neurol Neurosurg. 2013;115(8):1220-5. [Google Scholar] [Crossref]
- Halperin EC, Wazer DE, Perez CA, Brady LW. Principle and Practice of Radiation Oncology. 7th Edn.. . 2019. [Google Scholar]
- Kurwale NS, Suri V, Suri A. Predictive factors for early symptomatic recurrence in pilocytic astrocytoma: does angiogenesis have a role to play?. J Clin. 2011;18(4):472-7. [Google Scholar] [Crossref]
- Dirven CM, Mooij JJ, Molenaar WM. Cerebellar pilocytic astrocytoma: A treatment protocol based upon analysis of 73 cases and a review of the literature. Childs. 1997;13(1):17-23. [Google Scholar] [Crossref]
- Stuer C, Vilz B, Majores M. Frequent recurrence and progression in pilocytic astrocytoma in adults. Cancer. 2007;110(12):2799-808. [Google Scholar] [Crossref]
- Mclaughlin JE. Juvenile astrocytomas with subarachnoid spread. J Pathol. 1976;118(2):101-7. [Google Scholar]
- Bian SX, Mcaleer MF, Vats TS, Mahajan A, Grosshans DR. Pilocytic astrocytoma with leptomeningeal dissemination. Childs Nerv Syst. 2013;29(3):441-50. [Google Scholar]
- Pollack IF, Hurtt M, Pang D, Albright AL. Dissemination of low grade intracranial astrocytomas in children. Cancer. 1994;73(11):2869-78. [Google Scholar]
- Munshey A, Moore J, Maclean C. Cranial Pilocytic Astrocytoma With Spinal Drop Metastasis in an Adult: Case Report and Literature Review. World Neurosurg. 2017;98:883.e7-e12. [Google Scholar] [Crossref]
- Soliman RK, Budai C, Mundada P. Suprasellar pilocytic astrocytoma in an adult with haemorrhage and leptomeningeal dissemination: case report and review of literature. Radiol Case Rep. 2016;11(4):411-8. [Google Scholar]
- Drobysheva A, Klesse LJ, Bowers DC. Targeted MAPK Pathway inhibitors in Patients With Disseminated Pilocytic Astrocytomas. J Natl Compr Canc Netw. 2017;15(8):978-82. [Google Scholar]
How to Cite This Article
Vancouver
Keshri SK, Sinha SN. Intracranial pilocytic astrocytoma with spinal drop metastasis: A case review, discussion of its current management and related literature [Internet]. IP Indian J Anat Surg Head Neck Brain. 2021 [cited 2025 Oct 02];7(4):129-132. Available from: https://doi.org/10.18231/j.ijashnb.2021.033
APA
Keshri, S. K., Sinha, S. N. (2021). Intracranial pilocytic astrocytoma with spinal drop metastasis: A case review, discussion of its current management and related literature. IP Indian J Anat Surg Head Neck Brain, 7(4), 129-132. https://doi.org/10.18231/j.ijashnb.2021.033
MLA
Keshri, Shekhar Kumar, Sinha, Satyendra Narayan. "Intracranial pilocytic astrocytoma with spinal drop metastasis: A case review, discussion of its current management and related literature." IP Indian J Anat Surg Head Neck Brain, vol. 7, no. 4, 2021, pp. 129-132. https://doi.org/10.18231/j.ijashnb.2021.033
Chicago
Keshri, S. K., Sinha, S. N.. "Intracranial pilocytic astrocytoma with spinal drop metastasis: A case review, discussion of its current management and related literature." IP Indian J Anat Surg Head Neck Brain 7, no. 4 (2021): 129-132. https://doi.org/10.18231/j.ijashnb.2021.033
