Introduction
Lesions of the jaw range from benign to benign aggressive to malignant etiologies. They can be cysts, cyst-like lesions or tumors. Imaging plays a vital role in narrowing down the list of possible differential diagnoses. A systematic approach is essential to provide a meaningful diagnosis for each patient. These lesions can broadly be divided into radiolucent, mixed, or radioopaque based on their appearance on radiography which is the most widely used preliminary imaging modality in these cases. Some radioopaque lesions may be lucent, to begin with. Some of the most important questions to ask while radiological evaluation of these lesions include: What is the attenuation? What is the relation to the adjacent tooth? How are the margins (narrow/wide zone of transition)? Is perilesional halo present or absent? Whether there is bone expansion? The demographic distribution and associated clinical features add valuable information in arriving at a provisional working diagnosis. With the development of advanced imaging techniques, the role of the radiologist is on the rise not only in reaching the diagnoses but also in guiding the management. This review article aims to make the radiologists familiar with the commonly encountered jaw lesions and help develop a systematic approach for the evaluation of these lesions.
Approach to Lesions of Jaw
In the evaluation of jaw lesions, some basic observations are essential to be made.
The first question to be answered is whether a lesion is radiolucent, mixed or radio-opaque. The lesion may be lytic, sclerotic, mixed or may have ground-glass attenuation.
The second question is whether the transition zone between normal and abnormal bone is narrow or wide. The benign, slow-growing lesions have a narrow transition zone whereas aggressive lesions have a wide transition zone.
The third question is whether the lesion is related to a tooth (ie, it is intimately associated with a single tooth and in a tooth-bearing area of the jaw). Lesions which surround a component (eg, the crown or apex) of the tooth are usually, but not always, odontogenic in origin. If the lesion is not tooth-related, it usually indicates a lesion of osseous origin.
Odontogenic versus non-odontogenic lesions
Odontogenic lesions usually occur about a component of the tooth. A tooth-related lesion may also arise or persist at the site of a congenitally absent or extracted tooth. For example, radicular cysts grow around the tooth apex while dentigerous cysts surround the tooth crown. Non-odontogenic lesions usually have either no relation to teeth or may involve a large part of the bone near two or more teeth. While odontogenic lesions are usually seen above the inferior alveolar canal level, lesions below the level of the canal are non-odontogenic in origin. 1
The list of differential diagnoses of jaw lesions has been listed in Tables Table 1, Table 2, Table 3, Table 4, Table 5. Their clinical and demographic highlights, imaging features, management options, and prognoses have been discussed in detail later in this article.
Table 1
Radiolucent jaw lesions with a narrow zone of transition
Table 2
Radiolucent jaw lesions with a wide zone of transition
Table 3
Radio-opaque sclerotic lesions of Jaw
|
Odontogenic lesions |
|
|
• Periapical |
Cementoblastoma |
|
|
Cemento-osseous dysplasia |
|
|
Condensing osteitis |
|
• Pericoronal |
Odontoma |
|
Non- Odontogenic lesions |
|
|
|
Idiopathic osteosclerosis |
|
|
Osteoma |
|
|
Exostoses, tori |
Table 4
Radio-opaque ground-glass attenuation lesions of Jaw
Table 5
Mixed lytic- sclerotic lesions of Jaw
|
1. Osteonecrosis |
Osteoradionecrosis |
|
|
Medication-related osteonecrosis of jaw [MRONJ]). |
|
2. Osteomyelitis |
|
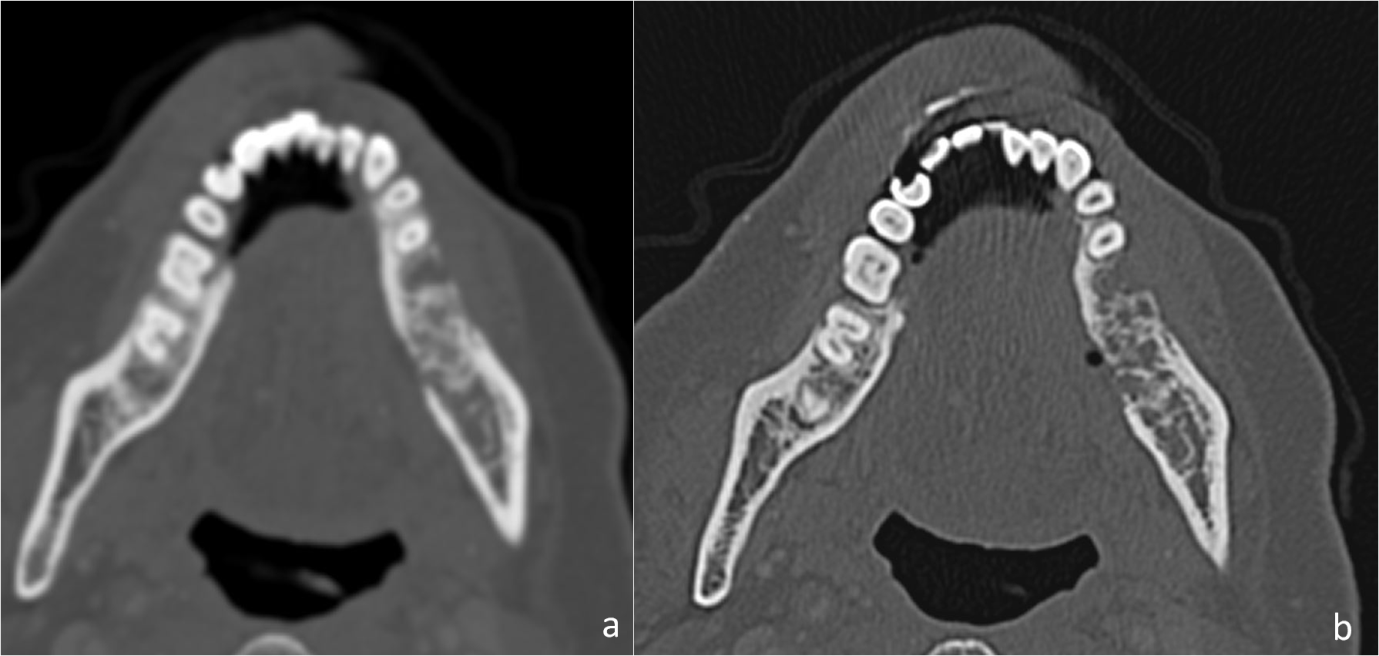
Figure 1
Axial CT scan images with soft tissue; (a): and bone window; (b,c): settings of a 25-year-old male with left mandibular swelling for 1 year shows an expansile unilocular cystic lesion causing cortical thinning involving posterior body of left hemi-mandible, displacing the last molar tooth. No soft tissue component or periosteal reaction was present. Histopathological analysis confirmed dentigerous cyst.

Figure 2
Axial contrast enhanced CT scan images with soft tissue; (a): and bone window; (b): settings of a 19-year-old male with left mandibular swelling for 5 months shows an expansile multiloculated cystic lesion involving posterior body and ramus of left hemimandible with enhancing soft tissue component within; a: Histopathological analysis revealed Ameloblastoma.
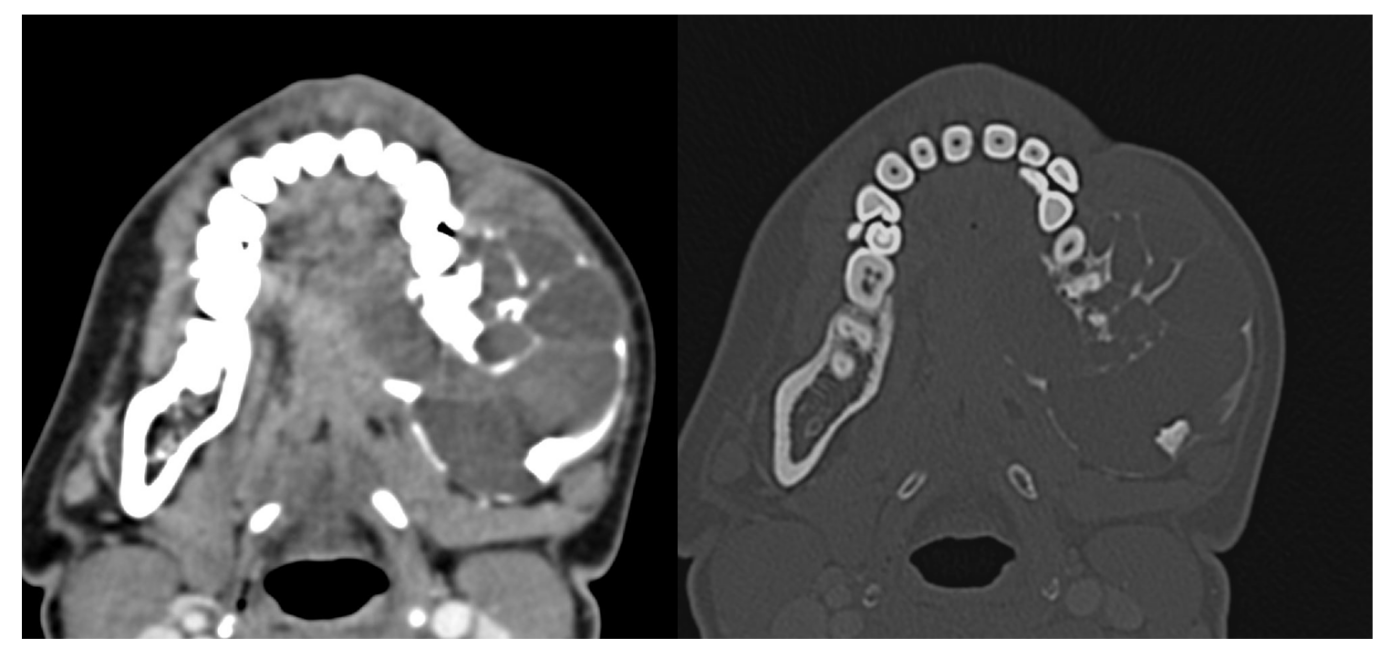
Figure 3
Axial CT scan images with bone window; (a,b,d): and soft tissue; (c): settings of a 3-year-old boy, known case of Langerhans Cell Histiocytosis, with swelling and pain in the jaw since 2 months showing multiple lytic lesions involving the body of bilateral hemi-mandible and skull base.
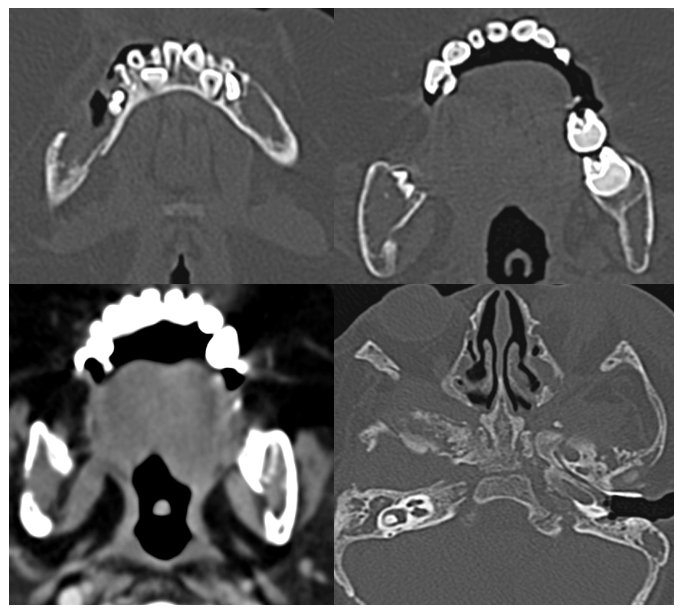
Figure 4
Axial T1; (a): T2; (b): and coronal T1 post-contrast MRI images; (c): of a 58-year-old male with known metastatic lung cancer, presenting with painful mandibular swelling for 2 months, show T1; (a): and T2; (b): intermediate signal soft tissue lesion involving left hemi-mandible with post-contrast enhancement; (c): Histopathological analyses confirmed metastases to the mandible.
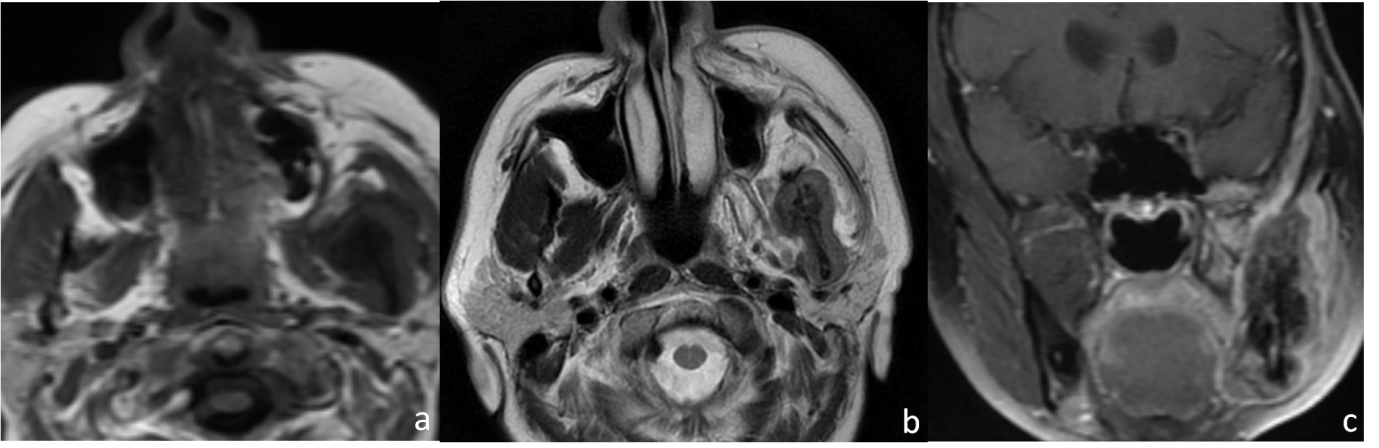
Figure 5
T1(a): T2(b): and post-contrast T1(c): axial MRI images of a 63-year-old male, a known case of multiple myeloma, with left mandibular swelling for 2 months show T1 and T2 intermediate signal lesion in left hemi mandible which shows mild post-contrast enhancement.
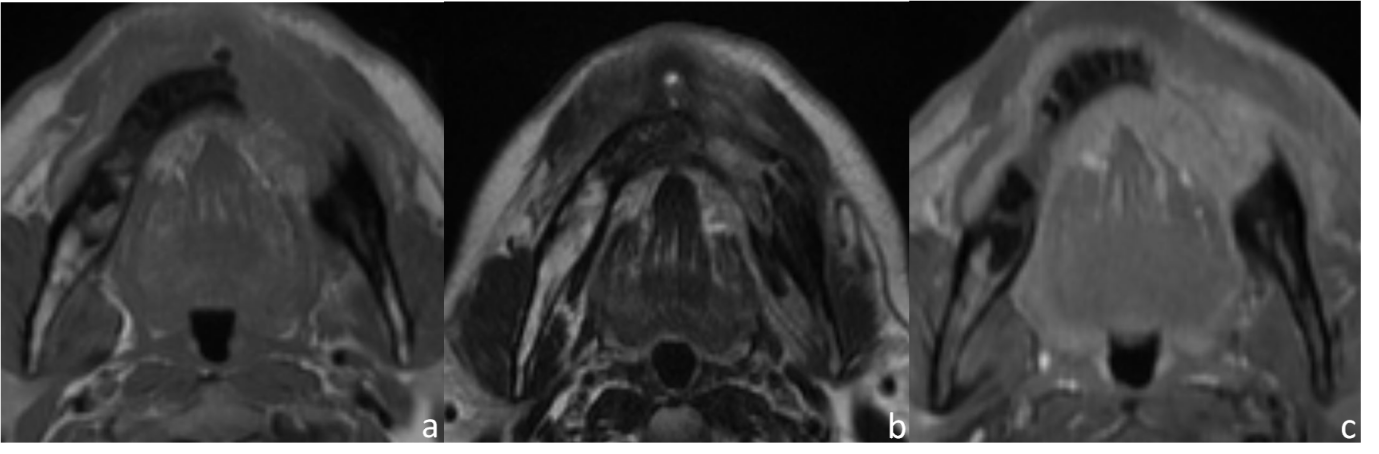
Figure 6
Axial soft tissue (a): and bone window (b): CT images of a 23-year-old woman with complaints of painful right mandibular swelling for 3 months and spontaneous loss of teeth show an expansile lytic lesion involving hemi-mandibular right body, ramus and condyle with sunburst pattern of periosteal reaction. Histopathological analyses revealed osteosarcoma.
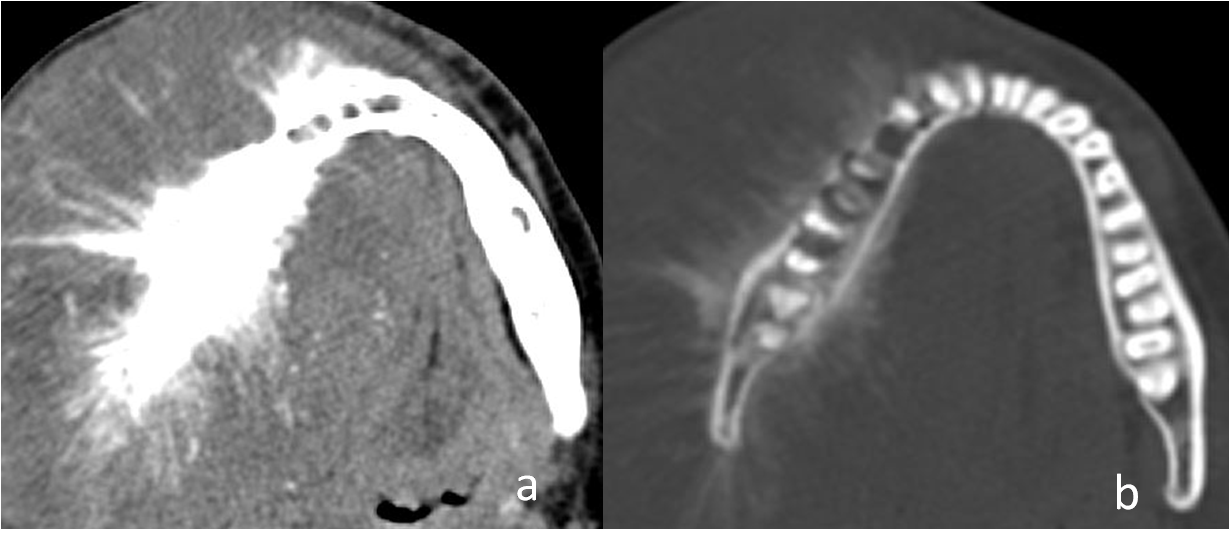
Figure 7
Axial T1 (a): T2 (b): coronal STIR (c): and post-contrast coronal T1 (d): MRI images of an 11-year-old male with a history of gradually increasing painful swelling of the left mandible since 1 month, with difficulty in chewing and mouth opening past 20 days shows T1 hypointense; T2 intermediate; STIR hyperintense; lesion in the ramus of left hemi-mandible with associated soft tissue component in the masticator space. It shows avid heterogeneous enhancement; Histopathological analyses revealed alveolar rhabdomyosarcoma of the mandible.
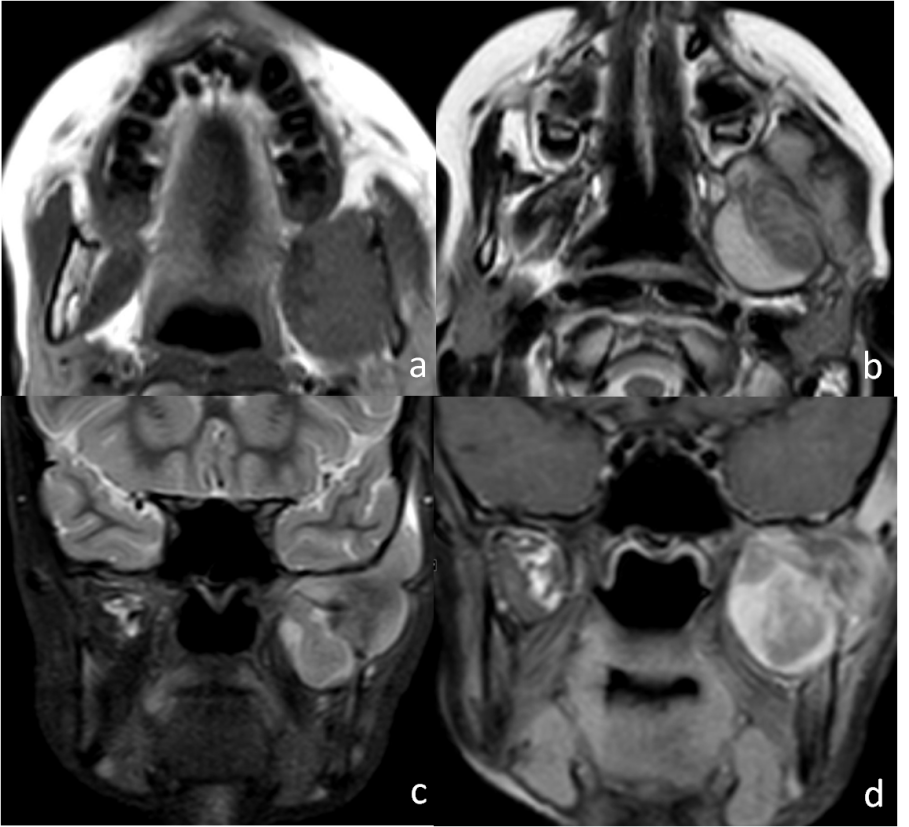
Figure 8
A 33 year old male presented with gradually progressive left mandibular swelling, bone window of axial and coronal CT images; (a,b): show a well-defined, left mandibular expansile lesion with dense sclerotic centre surrounded by radiolucent halo and a contour bulge. Radiological findings favour a complex odontoma.
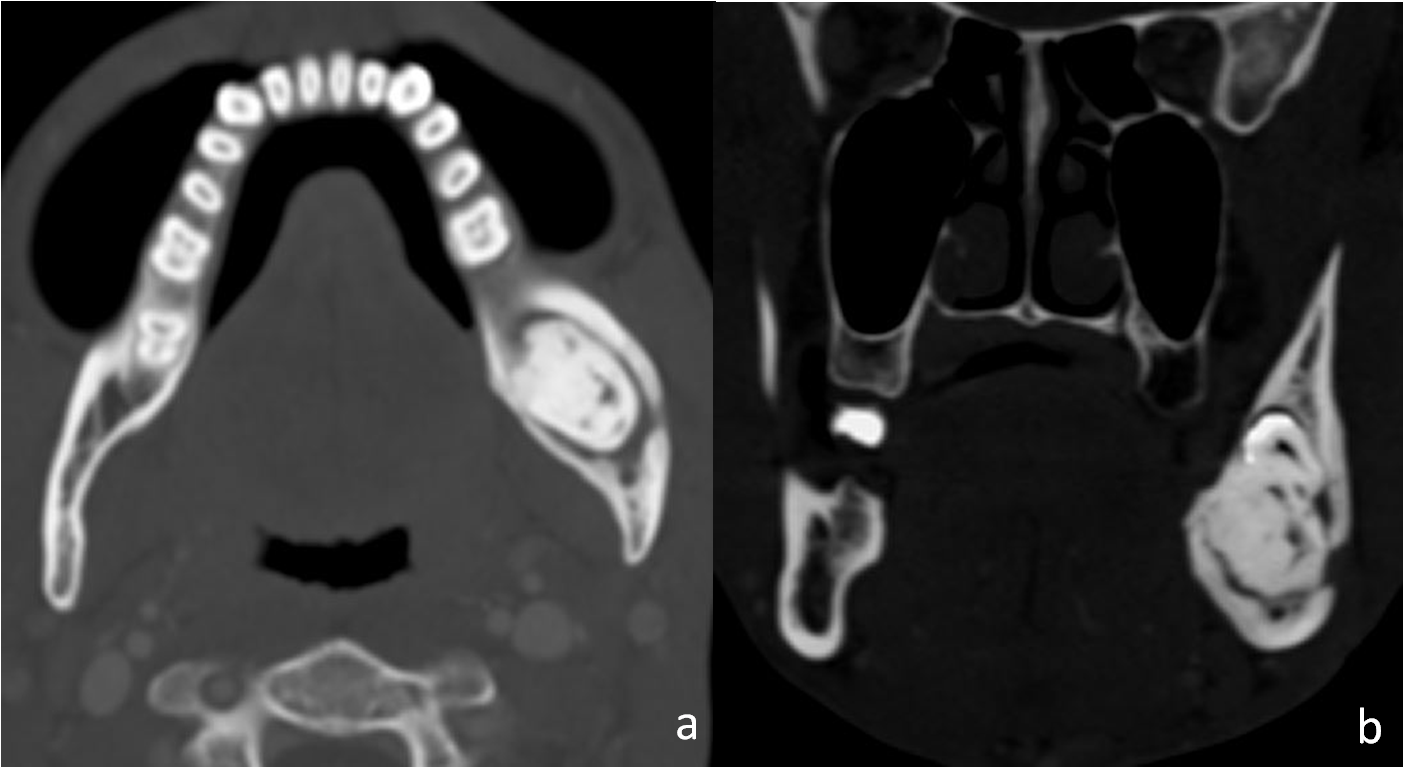
Figure 9
Axial CT scan images with soft window; (a): and bone window; (b): settings of a 12-year-old boy with right jaw swelling and pain since 5 months and difficulty in chewing, shows a well-defined, expansile lesion causing cortical thinningin the right ramus of the mandible. No hypodense halo seen. It closely abuts last molar tooth. Histopathology revealed ossifying fibroma.
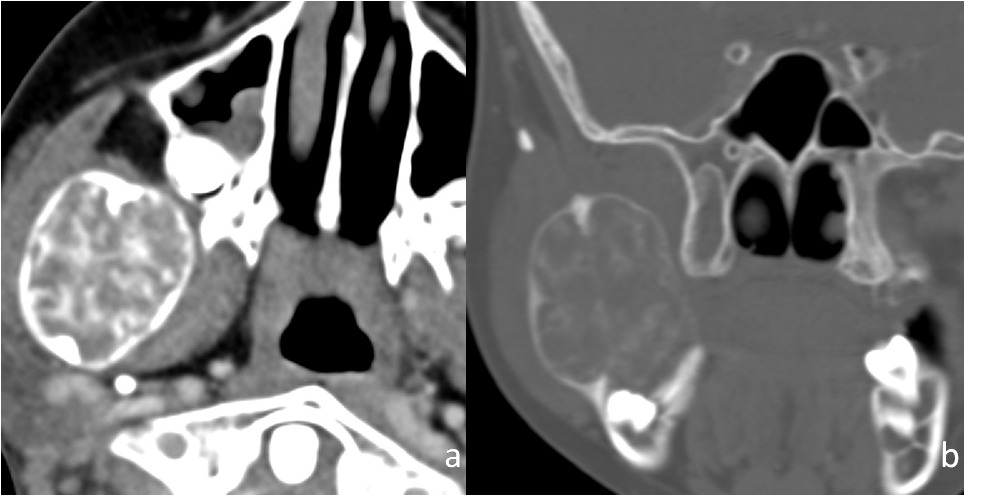
Figure 10
T1 axial (a): T2 sagittal (b): and coronal post contrast T (c): MRI sequences of a 20-year-old male with known history of chronic renal failure with renal osteodystrophy and on dialysis past 6 years, presented with painful right cheek swelling for 6 months, shows an expansile right maxillary lesion protruding into nasal cavity It appears hypointense on T1W; (a): with few hyperintense areas and intermediate on T2W; (b): and shows heterogenous post contrast enhancement; (c): PTH levels were elevated (619 pg/ml) and histopathological analysis supported the diagnosis of Browns tumor.
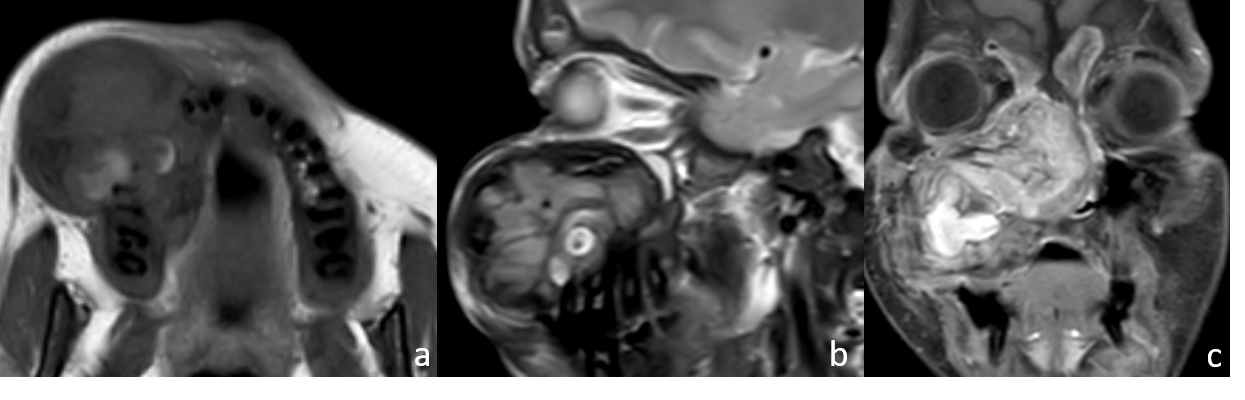
Figure 11
Axial soft tissue.(a): and bone window; (b): CT images of a 48-year-old woman with history of left buccal mucosal carcinoma, post-radiation therapy status, shows left mandibular lesion with permeative lytic destruction of mandibular alveolus with increased trabecular markings and cortical erosion. The clinico-radiological features suggested osteoradionecrosis.
Modalities for Imaging of Jaw lesions
Radiographs
The orthopantomogram (OPG) is the first investigation performed for a suspected jaw lesion. OPG gives us a complete view of the entire jaw and helps in determining the relation of the lesion with adjacent structures and teeth. However, the spatial resolution of OPG is inferior to that of intraoral radiography. 2 Since radiographs can give only a two-dimensional estimation. Nevertheless, radiographs play important role in the evaluation of margins and matrix of the lesion. More advanced imaging is, on most occasions, required to assess the detailed morphological characteristics of most of these lesions except radicular cysts which can be diagnosed on radiographs alone.
Computed tomography
For evaluation of both the osseous as well as the soft-tissue involvement of the disease Computed tomography (CT) is a better imaging tool. Excellent detail of lesion size, margins, matrix, and relationship to the inferior alveolar canal can be acquired using reconstruction on the bone window. OPG-like image can be obtained using panoramic reconstruction on multidetector CT (MDCT) which can aid in evaluating the relationship of the lesion to adjacent teeth whether they are merely displaced or eroded. The relationship of the lesion with the inferior alveolar canal and maxillary antrum can also be determined well on CT. Preoperative implant assessment requires orthoradial reconstructions of the jaw using CT. Evaluation of the soft-tissue window with the post-contrast study is useful in jaw infections and tumors. Cone-beam CT uses a low dose and provides a very high spatial resolution for further evaluation of osseous lesions. However, the time required to acquire the scan is higher. Detailed extraosseous assessment is not possible with this technology. 2
Magnetic resonance imaging
Magnetic resonance imaging (MRI) is an advanced imaging tool that helps better characterize the soft-tissue component of the lesion.MRI is a more sensitive modality to differentiate cysts from solid tumors. MRI Sequences including T1, T2, Diffusion-Weighted Imaging (DWI) and postcontrast T1(T1PC) are helpful in the evaluation of these lesions. DWI can help differentiate odontogenic keratocyst (OKC) from cystic ameloblastoma. 3 Marrow involvement is better assessed with MRI than CT, while CT is more useful for cortical involvement and detection of calcification.
Radiolucent Lesions with a Narrow Zone of transition
Odontogenic cysts
Radicular cyst -
It is the most common type and is often related to the root of a non-vital tooth. Tooth infection spreads to the pulp which forms periapical granuloma and abscess which gets epithelialized. These cysts are seen in the third to fifth decade of life and are usually asymptomatic. They are mostly less than 1 cm in size, with well-defined cystic lesions with a thin sclerotic rim. These cysts are seen around the root apex of a carious tooth, particularly the upper lateral incisor- a feature which helps differentiate it from apical periodontitis. Tooth resorption and displacement of adjacent roots can occur if the cyst is large. Treatment involves extraction and cyst wall enucleation.4
Residual cyst -
These are inflammatory cysts and are usually asymptomatic. These are seen on a post-extraction site. On imaging, they appear as well-defined cystic lesions with thin sclerotic rim and size usually less than 1 cm. Missing overlying tooth is a common association. These cysts are usually asymptomatic and do not require intervention. 5
Dentigerous Cyst (Follicular Cyst) (Figure 1) -
These are the most common non-inflammatory cystic lesion of the jaw and are commonly seen in young adults and adolescents. These are usually asymptomatic. On imaging, these are well-defined unilocular round/ovoid cystic lesion with smooth margins and surrounds the crown of an unerupted/impacted tooth, usually the third molar. These are formed when fluid accumulates between the unerupted/impacted tooth and the epithelium of the dental follicle that surrounds the tooth. The crown of the tooth projects within the cyst and the roots lie outside. Cysts which are larger than 2 cm in size may cause bone expansion, although the cortex is mostly preserved. There is no soft tissue or periosteal reaction. Larger cysts may have the potential to displace or resorb adjacent teeth. On MRI, these are hypointense on T1 (or maybe hyperintense due to proteinaceous contents), hyperintense on T2 and have a thin enhancing rim on post-contrast T1 images. Treatment of enucleation and curettage with the extraction of the involved tooth. Complications include the development of secondary mural ameloblastoma and rarely odontogenic carcinoma within a dentigerous cyst. Imaging features like bone erosion, enhancing solid nodules, or invasion of surrounding soft tissues may indicate the development of ameloblastoma within a dentigerous cyst. 4, 6, 7
Odontogenic keratocyst (OKC) -
It is common in the second to fourth decades of life. OKC is lined with odontogenic para keratinizing squamous epithelium and thin fibrous wall and has cheese-like contents within. These are more aggressive than other odontogenic cysts, as there occurs basal layer budding and formation of daughter cysts outside the primary cyst. These are associated with unerupted or impacted teeth. When these cysts are large, they can envelop the entire tooth and not just the crown. Basal cell nevus syndrome (Gorlin–Goltz syndrome) is known to present with multiple OKCs. On imaging, these are unilocular/multilocular cystic lesions, commonly seen in the posterior body and ramus of the mandible. These are well-defined and corticated and show expansion along the axis of the mandible with relatively little expansion along the buccolingual axis. On MRI, OKC shows an intermediate-to-high signal on T1, low-to-high signal (owing to keratinaceous contents)on T2 and thin or thick rim enhancement on post-contrast T1. Diffusion restriction is seen on DWI due to proteinaceous contents.
The closest differential diagnoses of OKC include-
Primary osteomyelitis- Cyst causes expansion of the involved jaw which is absent in osteomyelitis
Ameloblastoma- OKC shows expansion along the axis of the mandible with relatively little expansion along the buccolingual axis. Ameloblastoma shows buccolingual expansion.
Treatment includes enucleation with wide bony margin resection. This is the surgical method of choice as these are aggressive cysts with daughter cysts outside the primary lesion. A higher recurrence rate is associated with enucleation and curettage. If there is soft-tissue extension into orbit or masticator space, surgical excision may become extremely difficult. 3, 8, 9, 10
Non- odontogenic cysts
Stafne cyst/static bone cyst -
It is a pseudocyst of the mandible. It commonly involves the angle of the mandible posterior to the third molar tooth. It results from an aberrant submandibular gland or fat resulting in bowing and remodelling of the lingual cortex. A thin sclerotic rim is present all around the cyst. These cysts are present below the level of the inferior alveolar canal as they are non-odontogenic. They are usually picked up as incidental findings and require no treatment. 11
Simple bone cysts -
These are also known as solitary/traumatic/haemorrhagic bone cysts. These are pseudocyst with no epithelial lining. These cyst formation form results following trauma from intramedullary haemorrhage. These are usually asymptomatic and common below 20 years of age. A male predominance is seen. These are commonly seen in the posterior mandible. On imaging, these are unilocular cysts that may have expansile, scalloped margins. Haemorrhagic contents can be seen well on both CT and MR. No post-contrast enhancement is seen. Treatment is usually by curettage. Only, when it cannot be distinguished from other cysts like OKC, surgical exploration may be necessary. 4, 11
Nasopalatine cyst -
These cysts originate from the remnant epithelium of the nasopalatine duct which usually regresses in fetal life. These are also called midline maxillary cysts, anterior midline palatine cysts, or incisive canal cysts. These are more common in men in their fourth and fifth decades of life. These are mostly asymptomatic but can cause pain and discharge if the cyst gets infected. On imaging, these are seen as round to ovoid well-defined corticated lesions above the roots of the central incisors. These cause divergence of roots of teeth. These can assume a “heart shape” in some cases, due to the central nasal spine. Treatment is usually by enucleation if the cyst is symptomatic. 12
Odontogenic solid lesions
Ameloblastoma (Figure 2) -
These are the most common odontogenic tumour amounting to nearly 10% of such tumors. Ameloblastoma arises from the enamel forming cells of the odontogenic epithelium and less commonly from the lining of a dentigerous cyst and is locally aggressive. These are common in the fourth to sixth decades of life and show no sex predilection. These may be incidental or present as painless jaw swelling. The WHO 2017 fourth edition classification of head and neck tumors classifies ameloblastoma into ameloblastoma, unicystic ameloblastoma, extraosseous/peripheral type, and metastasizing ameloblastoma. These are common in the posterior body and ramus of the mandible. On radiographs/OPG, they are radiolucent lesions. They are unilocular or multilocular and the presence of septations can give rise to a “honeycomb” or “soap bubble” appearance. These cause marked buccolingual expansion with cortical thinning/breach. The presence of cortical breach, root resorption, and soft-tissue extension indicates the aggressiveness of the lesion. On MRI, ameloblastoma has a low signal on T1, and a high signal on T2, the solid component shows restricted diffusion while the cystic component has facilitated diffusionon DWI. Enhancement of the solid component is seen on post contrast T1. The closest differential diagnosis is OKC. Ameloblastoma shows buccolingual expansion while OKC shows expansion along the axis of the mandible with relatively little expansion along the buccolingual axis.2, 7, 8, 10, 13, 14
Non-odontogenic solid lesions
Central giant cell granuloma -
These are also known as Giant cell reparative cyst or giant cell granuloma and result from a reactive process secondary to haemorrhage within the mandible. Areas of haemorrhage, fibrous tissue, and osteoclast-like giant cells can be seen within these lesions. These are common in young women in their second and third decades of life. Characteristic location is the anterior mandible or maxilla with a tendency to cross the midline. On imaging, these are seen as a well-defined, multilocular radiolucent lesions. Bone expansion, cortical thinning and remodelling are present. “Honeycomb” appearance may be seen due to internal septations. On MRI, the intermediate signal on T1, hypointense to intermediate signal (T2 shortening is due to haemorrhage and giant cells) on T2 and moderate to marked enhancement on post-contrast T1 is seen. The closest differential diagnoses include OKC, Ameloblastoma, and Brown tumor. Demographic features, location of the lesion, and laboratory findings can point toward the correct diagnosis. Treatment involves conservative methods like intralesional steroid injection, calcitonin injections, and radiotherapy are used for slow-growing lesions. Definitive treatment requires enucleation and curettage. Surgical resection may be done in aggressive cases. 2, 4, 15
Venous malformation -
These are common in women in the second to fifth decades of life and are mostly asymptomatic though may present as painless jaw swelling, mobile teeth, pain, and paraesthesia.These are common in the body of the mandible and have varied imaging appearances ranging from the unilocular cyst, cyst with ill-defined borders or sclerotic rim to the multilocular expansile lesion with honeycomb appearance resulting from fine trabeculae within the lesion. “Sunburst” appearance with radiating bone spicules and soap bubble/tennis racquet appearance in an expansile lesion with septations may be seen. The closest differential diagnoses include osteosarcoma when these present with a sunburst appearance and odontogenic myxoma when Tennis racquet appearance is present. A high index of suspicion is important in imaging for reaching the correct diagnosis as the lesion can have catastrophic bleeding. Needle aspiration should precede biopsy when this suspicion is raised. Treatment includes steroid therapy, sclerosing agents, radiotherapy, and surgical excision. Surgical intervention is the definitive treatment where the surgeon needs to be prepared to handle brisk intraoperative bleeding. 4, 16, 17
Langerhan cell histiocytosis (LCH) (Figure 3) -
LCH is characterized by abnormal proliferation of Langerhan cells in the reticuloendothelial system. The mandible is the second most common bone to be involved after the skull. Lesions of LCH are lytic with ill-defined borders in the early stage to well defined and sclerotic margins in the late phase of the disease. Cortical breach and periosteal reaction are present. Involvement of the alveolar crest can give rise to a “scooped out” appearance. “Floating teeth” appearance results from the destruction of the alveolar bone. On MRI, lesions are hypointense on T1, hyperintense on T2 and show marked enhancement on post-contrast images. The closest differential diagnoses include osteomyelitis and malignant lesions when ill-defined margins, cortical breach, and soft-tissue extension are seen. Treatment options include surgery, radiotherapy, chemotherapy, and intralesional injection of corticosteroids. The decision depends on the number, size, and location of lesions. 18, 19
Radiolucent lesions with a wide zone of transition
Odontogenic tumors
Malignant odontogenic tumors -
As per 2017 WHO classification of odontogenic lesions, these are rare tumors that include odontogenic carcinoma, odontogenic carcinosarcoma, and odontogenic sarcomas. These are more common in men in their sixth to eighth decades. These are seen as irregular ill-defined radiolucent lesions on radiographs. Ill-defined margins, cortical destruction, soft-tissue extension, MRI features include restricted diffusion and post-contrast enhancement within the solid component. Atypical features like well-defined smooth margins or a sclerotic rim may be seen. Treatment requires extensive resection with clear margins. 6, 14
Malignant non-odontogenic tumors
Squamous cell carcinoma (SCC) of the oral cavity -
Mostly affects men above the age of 50 years. Locally advanced disease can involve the mandible or maxilla. Imaging plays an important role in the staging of disease. Ill-defined lysis involving the bone adjacent to the oral cavity mass. Treatment includes surgery or a combination of surgery and chemoradiation.5
Metastases (Figure 4) -
Distant metastases to the mandible is more common than maxilla in the ratio of 4:1 due to the paucity of red marrow in the maxilla. The most common primary malignancies to metastasize to the jaw are lung, prostate (sclerotic metastases), kidney (hypervascular and expansile metastases), breast, gastrointestinal, and thyroid (expansile metastases) cancers. Metastases are common in the posterior body and angle of the mandible. On imaging, these lesions appear as ill-defined lytic lesions with no accompanying periosteal reaction. Treatment of these patients is essentially palliative as metastases are usually widespread when jaw metastases have occurred. 6, 11, 20
Hematological malignancy -
Leukemia, lymphoma and multiple myeloma can involve the jaws. Primary jaw lymphoma is usually Non-Hodgkin lymphoma. Lymphoma can present as ill-defined permeative lesions which on MR are seen as marrow infiltration. The involvement of soft tissues is more florid than cortical involvement. MRI features of lymphoma include a low-to-intermediate signal on both T1 and T2 weighted sequences with homogeneous post-contrast enhancement. Multiple accompanying enlarged nodes support the diagnosis of lymphoma. Multiple myeloma (Figure 5) presents as single or multiple punched out lesions with no rim, the ill-defined permeative pattern of bone destruction, or a large area of bone destruction. On MRI, the low–to-intermediate signal is seen on T1 and a high signal on T2. Treatment of haematological malignancies is primarily medical management. 2, 20
Sarcoma -
Include osteosarcoma (most common) [Figure 6], chondrosarcoma, fibrosarcoma, Ewing sarcoma and rhabdomyosarcoma (mainly in children) [Figure 7]. Osteosarcoma may also occur secondary to radiation therapy of the head and neck region. It is most often seen to involve the posterior mandible with a peak incidence in the third and fourth decades of life. It can present as lytic, sclerotic, or mixed aggressive lesion with periosteal reaction, bone destruction and adjacent large soft tissue. A characteristic feature of Osteosarcoma is the presence of an osteoid matrix. Sclerotic and mixed forms may have the characteristic “sunburst” periosteal reaction with cortical destruction. Ewings sarcoma has no matrix. It shows a multilamellar periosteal reaction. Chondrosarcoma has a cartilaginous matrix.Treatment involved resection if possible. Alternatively, radiotherapy and chemotherapy can be considered. 6
Malignant transformation of intra-osseous salivary epithelial remnants -
These tumoursarise from salivary epithelial rests within the jaw. Mucoepidermoid carcinoma of the mandible is an extremely rare variety. Women are nearly twice as commonly affected as men with a mean age of presentation in the fifth decade of life. These tumours present as a well-defined multilocular cystic mass or ill-defined lytic area. They are common in the angle or posterior body of the mandible. Medullary bone destruction with intact cortex is a characteristic feature. Cortical breach and soft-tissue extension maybe present. On MRI, a bright signal within the cystic component and a low signal within the solid component is seen on T2 with restricted diffusion within the solid component on DWI. The primary treatment is surgery. Neck dissection is usually done in cases with nodal metastases. Radiotherapy is given for high-grade tumors. 21
Radio-opaque sclerotic lesions of Jaw
Cementoblastoma
It is a rare benign periapical lesion. It makes up less than 1% of all odontogenic tumours and is most common in children and young adults. These are more common in the mandible and 90% develop in the molar or premolar region. They are associated with an erupted permanent tooth but they may be found near an impacted or unerupted tooth. At imaging, cementoblastomas appear as a periapical, sclerotic, well-defined lesion with a hypodense halo. They directly fuse to the root of the tooth 22. Treatment involves complete removal of the associated tooth to reduce the likelihood of recurrence. 23
Cemento-osseous dysplasia -
Formed as a result of a hamartomatous process that is usually associated with tooth apices. It typically arises in the anterior mandible where it involves one or only a few teeth. Another variety that occurs in the posterior jaw and involves molar teeth is called focal cemento-osseous dysplasia. Dull ache may be the only presentation. On imaging, early lesions are lytic, may appear mixed lytic and sclerotic later, and have a central area of calcification. Both late cementoblastoma and cemento-osseous dysplasia are periapical, sclerotic, well-defined lesions with a hypodense peripheral halo. However, cementoblastoma is seen in children and young adults whereas cemento-osseous dysplasia is common among black women and women of Asian descent who are in the 4th or 5th decade of life. Also, cementoblastoma fuses directly to the tooth root, whereas cemento-osseous dysplasia does not. 24, 25
Condensing osteitis -
It is seen in children and young adults and is more common in the mandible. The premolar and molar regions are commonly involved. It is a localized form of reactive osteitis and sclerosis that surrounds the apices of teeth with pulpitis or pulpal necrosis. The adjacent tooth usually may show a periapical inflammatory lesion like granuloma, cyst, or abscess. On imaging, a periapical, ill-defined, non-expansile, sclerotic lesion adjacent to the carious tooth is seen. It may be uni- or multifocal. 26
Odontomas (Figure 8) -
These are the most common odontogenic tumour. These are most commonly seen in children. They form a developmental anomaly (hamartoma) and may obstruct tooth eruption. Usually associated with an impacted tooth, although they may develop before or after tooth eruption. On imaging, pericoronal, well-defined, and sclerotic lesions, with a low-attenuation halo are seen. Early odontomas may appear purely lucent or may become expansile. These can be classified as simple, compound, or complex. Simple odontomas present as supernumerary teeth. Compound odontomas consist of multiple small tooth like structures called denticles and most commonly arise in the anterior maxilla. Complex odontomas are seen as a conglomerated mass of amorphous hyperdense enamel and dentin, most commonly in the molar regions. The closest differential diagnosis of a complex odontoma is an osteoma, the low-attenuation halo that surrounds the odontoma may help differentiate these lesions. 22, 27 Occasionally, odontoma is associated with dentigerous or calcifying odontogenic cysts. 24
Idiopathic osteosclerosis -
It is a focal solitary sclerotic lesion that arises in the late 1st or early 2nd decade of life. It is usually asymptomatic. There is typically no associated inflammation. Lesions may remain static or demonstrate slow growth that usually stops when the patient reaches skeletal maturity. It more commonly affects the mandible than the maxilla, usually near the first molar or second molar or premolar. On imaging, it is seen as small and round or oval, sclerotic, periapical, and tooth-related lesion with sharp margins with peripheral speculation. Rarely, It may not be related to a tooth. Idiopathic osteosclerosis is non-expansile and has no low-attenuation rim. 28, 29
Osteomas -
These are non-odontogenic bone lesions. Osteomas are benign. They are composed of mature compact or cancellous bone and are common in the craniofacial skeleton. The posterior mandibular body or condyle is commonly affected. Multiple osteomas may be seen in Gardner syndrome. 30 On imaging, osteomas appear as a non–tooth-related well- defined, expansile sclerotic mass with no perilesional halo. The closes differential diagnosis is idiopathic osteosclerosis when no bone expansion is present. 31
Tori and exostoses -
These are protuberances of dense cortical bone. These are common in adults. These usually manifest with no symptoms. Occasionally, they contain a small amount of marrow. They are characterized by slow growth that usually arrests spontaneously. Genetic and environmental influences play a role in their pathogenesis. 32
Jaw lesions with ground-glass attenuation
Ossifying fibroma (Figure 9)
This entity includes the following subtypes: ossifying fibroma, cemento-ossifying fibroma, and juvenile ossifying fibroma. There is a female predilection in the case of ossifying fibroma. These typically present as painless swelling around the mandible. The common sites involved are premolar and molar areas. Its highest incidence is seen in the 3rd and 4th decades of life. These neoplasms show centrifugal growth perpendicular to the long axis of the bone. Juvenile ossifying fibroma, especially the trabecular form, is aggressive and destructive and may arise in either the maxilla or mandible. On imaging, ossifying fibroma typically presents as a solitary, well-marginated, unilocular, expansile lesion. It has diffuse ground-glass attenuation with no hypodense halo. Occasionally, a sclerotic border may be seen. Ossifying fibroma appears radiolucent, to begin with, because of non-mineralized osteoid. Later, with the mineralization of the matrix, it becomes radio-opaque. Associated enhancing soft tissue may be seen, and tooth displacement and erosion are common. 33, 34
Fibrous dysplasia
These lesions cause diffuse enlargement with expansion along the longitudinal axis of the affected bone such that the original shape of the bone is maintained, with less focal alteration to its general shape as compared to ossifying fibromas. Fibrous dysplasia is made of cellular fibrous tissue and woven bone trabeculae. There is no osteoblastic rimming (unlike ossifying fibroma). The malignant degeneration of fibrous dysplasia typically involves the craniofacial region. Most craniofacial fibrous dysplastic lesions are monostotic. Craniofacial fibrous dysplasia, Lichtenstein-Jaffe fibrous dysplasia, and Albright syndrome are the three different types of polyostotic fibrous dysplasia. Craniofacial fibrous dysplasia only affects craniofacial bones. In the Lichtenstein Jaffe type of fibrous dysplasia, the polyostotic disease affects both craniofacial and noncraniofacial bones. Albright syndrome is characterized by cutaneous café au lait spots, severe polyostotic fibrous dysplasia (mostly unilateral), and endocrinopathies. At imaging, fibrous dysplasia is seen as ground-glass attenuating areas with a wide transition zone, a feature that helps differentiate it from ossifying fibroma. Its cortex remains intact and is often thickened and sclerotic. Other features that indicate fibrous dysplasia are non-displaced teeth and crossing of sutures. 33, 35
Renal Osteodystrophy (Figure 10)
It comprises a spectrum of bone diseases associated with renal insufficiency and secondary hyperparathyroidism. There is increased osteoclastic activity due to secondary hyperparathyroidism which develops in patients with chronic renal failure. Benign fibro-osseous lesions are more common in patients with renal osteodystrophy.Imaging mimics that of diffuse fibrous dysplasia as there is the replacement of normal trabeculation by areas of diffuse ground-glass attenuation and a loss of definition of the cortex, the lamina dura, and the wall of the inferior alveolar nerve canal. Osteitis fibrosa, a more advanced disease pattern is characterized by mixed osteolysis and sclerosis due tothe presence of bone resorption, osteoid production, and increased bone remodelling. Brown tumours (also known as osteitis fibrosa cystica) may be seen in patients with primary or secondary hyperparathyroidism. These are expansile and lytic lesions, which are typically hypervascular and may contain old haemorrhage. 33, 36, 37
Mixed lytic-sclerotic lesions of Jaw
Osteomyelitis
Develops secondary to periodontal infection, trauma, foreign body, or a prior surgical procedure and ismore common in the mandible than the maxilla. Acute osteomyelitis presents with severe pain, fever, swelling, trismus, paraesthesias, or even pathological fracture. Chronic cases are indolent in presentation. Imaging features on radiograph include indistinct cortex which becomes obvious only 1 to 2 weeks after onset of infection. Ill-defined lytic lesions in bone, permeative bone destruction, and periosteal reaction may be seen. Sequestrate (dense necrotic bone) is seen in chronic osteomyelitis. On CT/MRI, there is loss of surrounding soft-tissue fat planes and variable post-contrast enhancement of involved bone and adjacent soft tissues. Rim-enhancing abscesses can be seen. Treatment consists of antibiotics and surgical debridement. 4, 11
Osteonecrosis (Figure 11)
Osteonecrosis is the result of radiation (osteoradionecrosis) or medication that may have antiangiogenic/bone remodelling suppression effects (medication-related osteonecrosis of the jaw [MRONJ]). These medications include bisphosphonates, tyrosine kinase inhibitors and vascular endothelial growth factor (VEGF) inhibitors.
The diagnosis of MRONJ is based on three criteria as follows:
Area of exposed bone not healing for more than 8 weeks.
Past or current treatment with medications that can cause MRONJ.
No radiation therapy for head and neck regain.
MRONJ has been reported to occur between 6 and 60 months of treatment. Most cases of osteoradionecrosis are reported to occur within 4 months to 2 years. Diagnosis is primarily clinical. In the early stage of the disease, ill-defined lytic areas or permeative bone destruction with sclerosis are seen. In the advanced stage of the disease, however, sequestration, fragmentation, areas of gas attenuation, cortical destruction, periosteal reaction, and pathological fractures may be seen. Variable signal intensity can be seen on both T1W and T2W images with variable contrast enhancement depending on the marrow oedema, marrow sclerosis, and sequestrum seen in different stages of the disease on MRI. The closest differential diagnosis includes Osteomyelitis and malignant involvement by primary or secondary neoplasm. Superimposed infection can be considered ifan abscess is present. DWI imaging can also help in the differentiation of osteonecrosis from neoplastic pathology. Treatment is mainly conservative with oral care, treatment of superadded infection, and pain control. Surgery is usually not the primary treatment modality, as it may aggravate necrosis but may be considered in nonresponsive cases. 6, 38, 39, 40
Conclusion
Lesions of the jaw range from benign to benign aggressive to malignant etiologies. These can be odontogenic or non-odontogenic. Imaging plays a vital role in narrowing down the list of possible differential diagnoses. A systematic approach is essential to provide a meaningful diagnosis for each patient.

