Introduction
Nasal obstruction compromises the quality of sleep when it results in breathing disorders and fragmentation of sleep, as per current belief. But majority of studies have failed to objectively associate sleep quality and nasal obstruction. 1 Nasal obstruction might be congenital or acquired at some point during a lifetime. It may be a result of a structural change in the nasal cavity or it may arise due to nasal congestion.2 Structures of the nose that are areas of special concern are internal nasal valve, the septum and the choana. The nasopharynx is particularly important in children, because hypertrophied adenoids are the cause of obstructive sleep apnoea (OSA). 3 The adult nasopharynx with lymphoid hypertrophy in lateral and posterior wall plays important role in causing obstruction of the airway.
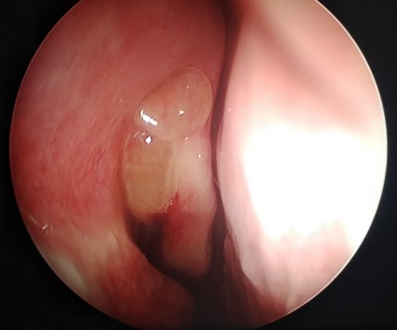
Examination of the nasal and nasopharyngeal airway is essential for patients in whom obstructive sleep apnoea (OSA) is suspected or is diagnosed. It helps in determining an optimal treatment. Nasal examination by anterior rhinoscopy allows evaluation of anterior septal deviation, internal nasal valve angle, and inferior turbinate size. Frequently, this limited examination of the anterior nasal cavity does not correlate with patient symptoms. Patients may complain of nasal obstruction despite no signs of anatomical abnormalities in the nasal cavity in anterior rhinoscopy. Structural and inflammatory problems often coexist and need to be addressed concurrently in order to evaluate normal nasal function. 4 Other aetiologies for nasal obstruction such as posterior septal deviation or chronic sinusitis with or without polyposis may go undiagnosed. And these can be evaluated with the help of Posterior rhinoscopy and Nasal endoscopy. Nasal endoscopy is essential to visualize the site and degree of nasal and nasopharyngeal obstruction, as some areas are difficult to assess by nasal examination alone.
Numerous observational studies have demonstrated that nasal congestion is associated with snoring and daytime sleepiness. A threefold increased incidence of snoring and daytime sleepiness in volunteers with self-reported nocturnal nasal congestion,5 while polysomnography and rhinomanometry showed a correlation between nasal resistance in the supine position and habitual snoring. 6 Many variables are involved in the pathogenesis of the disease, making the choice of the correct treatment a complex one.
Data on OSA patients treated for nasal obstruction alone has shown consistent improvement in subjective symptoms such as daytime somnolence and snoring despite minimal change in their sleep study results.7 Nasal surgery alone has also been shown to significantly impact CPAP tolerance and adherence. 8
Obstructive Sleep Apnoea is defined as apnoea secondary to airway collapse with subsequent blockage of the upper airway during sleep. Traditionally, night time Polysomnography (PSG) in an attended setting (sleep laboratory) has been used as a reference standard for the diagnosis of OSA. Polysomnography measures several sleep variables, one of which is apnoea-hypopnea index (AHI).
The AHI has been widely used to diagnose OSA, although with different cut off levels9 -
In adults
In children- Very mild-1-5
An abnormal AHI accompanied by excessive daytime sleepiness is the hallmark for OSA. Daytime sleepiness is measured using Epworth Sleepiness Scale (ESS). 10
Based on above background, nasal and nasopharyngeal obstruction appears to play an important role in causation of obstructive sleep apnoea. We aim to find the incidence of nasal and nasopharyngeal obstruction, by clinically examining the nasal cavity and nasopharynx and performing nasal endoscopy, who are diagnosed to have obstructive sleep apnoea by Polysomnography and to correlate the levels of nasal and nasopharyngeal obstruction with degree of OSA.
Materials and Methods
Sampling design
Patients with complaint of snoring & having abnormal polysomnography attending ENT OPD at JLN Main Hospital & Research Centre, Bhilai, Chhattisgarh. Patients with abnormal polysomnography referred from other departments.
Estimated sample size
80 Patients. Calculation- From previous study- Torre C, Capasso R, Zaghi S, Williams R, Stanley Y. High incidence of posterior nasal cavity obstruction in obstructive sleep apnoea patients. Sleep Science and Practice 2017. 2017;1. 8
P= posterior nasal obstruction findings in OSA patients = 26.6%
96= Z value for 5% confidence level
e= precision= 0.10
Cochran formula for descriptive analysis
Minimum sample size (n) =
= (3.8416*0.266*0.734)/ (0.10)2 =75
Minimum sample size = 75 OSA patients
To increase power and reliability of the study we are going to take the sample size as 80.
Inclusion criteria
Patients willing to take part and give written informed consent, Patients with complaints of snoring, attending department of ENT irrespective of sex in adults of all age group, with abnormal polysomnography and Patients referred from other departments with abnormal polysomnography.
Exclusion criteria
Patients not giving consent for our study. Patients with AHI < 5, Paediatric patients, Pregnant patients, Patients on sedative medications & psychiatric patients, Patients who have undergone previous nasal & nasopharyngeal surgery, Critically ill patients and patients with Craniofacial anomalies.
Methodology
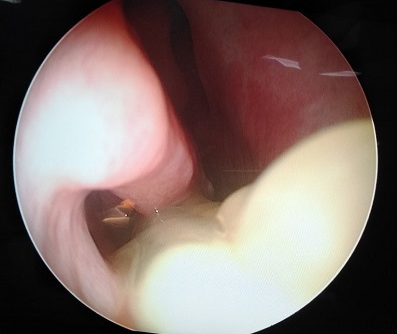
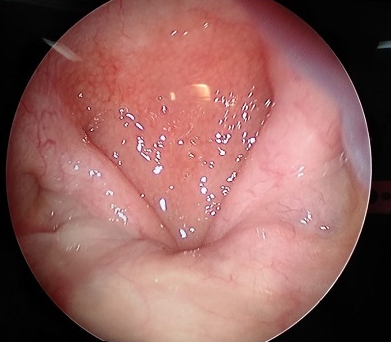
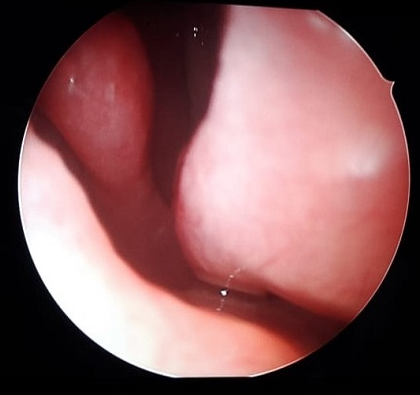
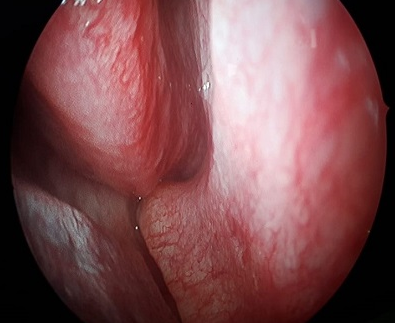
Ethical clearance to conduct the research was obtained from ethical review committee (ERC) as per national ethical guidelines. The patients those presented in OPD with snoring, with abnormal polysomnography and those referred from other departments with abnormal polysomnography were selected. Polysomnography was done by RMS Quest 32 polysomnography machine. Written informed consent (form attached) from the patient or guardian/relatives before Clinical and nasal examination and Nasal Endoscopy. History taken in detail regarding- Age, Sex, Snoring, Apnoeic spells, Daytime sleepiness, Nasal obstruction and other medical conditions, surgical history as per study proforma. General clinical examination for BMI and Neck circumference was done. Nasal Examination to visualise the site of nasal obstruction by anterior and posterior rhinoscopy. Anterior rhinoscopy using Thudicum’s nasal speculum and Posterior rhinoscopy using posterior rhinoscopy mirror while Nasal endoscopy to visualise nasal and nasopharyngeal airway for obstruction using 0o Hopkin’s rod endoscope under topical anaesthesia using 4% Xylocaine. Analysis of data and calculation of incidence of nasal and nasopharyngeal obstruction in patients with abnormal polysomnography.
Observation and Results
Age distribution
Maximum number of patients in our study belonged to 51 to 60 years of age group. Oldest patient is 80 years old and the youngest patient is 27 years old.
BMI distribution
Maximum patients in our study group were in obese category with BMI range 30 kg/m2 to 39.9 kg/m2. One of the patients was in underweight category with BMI 17.9 kg/m2 and 7 patients had BMI between 23 kg/m2and 24.99 kg/m2 i.e. overweight category. None of the patients in our study group had normal BMI.
Neck circumference distribution
Percentage of patients with larger neck circumference was more among females (83.33%) than in males (42.86%).
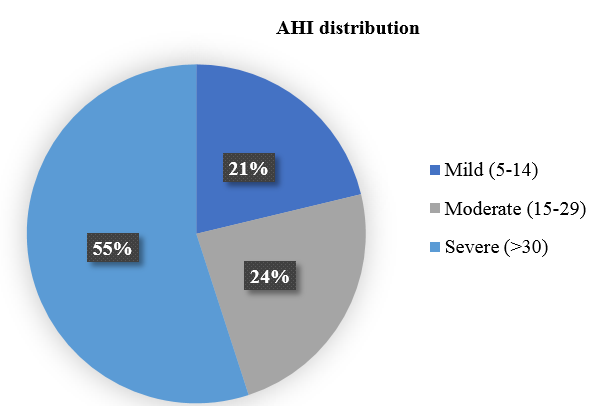
Severity of obstructive sleep apnoea distribution
55% patient had Severe OSA with AHI >30. 21.25% had mild while 23.75% had moderate OSA. Mean AHI of patients mild OSA was 9.49, moderate OSA 22.52 and Severe OSA was 53.13. (Figure 7)
Anterior rhinoscopy findings distribution
In anterior rhinoscopy examination, we found 31 patients had deviated nasal septum and 19 had hypertrophied turbinates. 4 patients had Chronic Rhinosinusitis with Nasal Polyposis.
Posterior rhinoscopy findings distribution
21 Patients had posterior DNS on posterior rhinoscopy examination and 7 patients had postnasal drip.
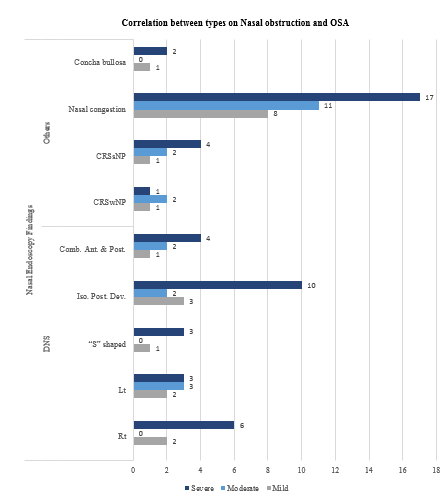
Distribution of types of nasal obstruction by nasal endoscopy
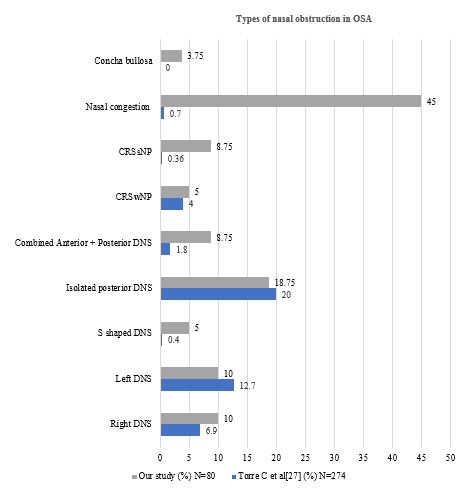
Mucosal inflammation was the most common finding on nasal endoscopy of our patients. Total 42 patients that Deviated nasal septum among which 20 had anterior and 15 had posterior deviation. 7 patients had both anterior and posterior DNS. 4 patients had CRSwNP while 7 had CRSsNP. 3 patients had concha bullosa.
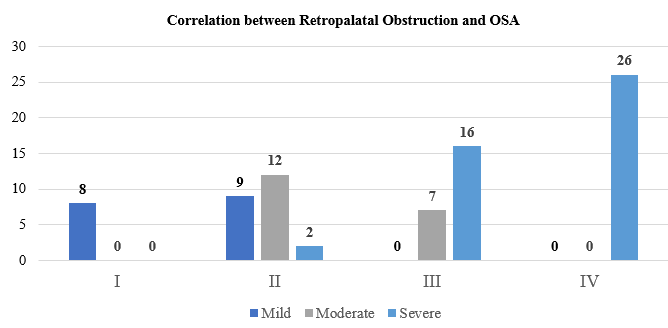
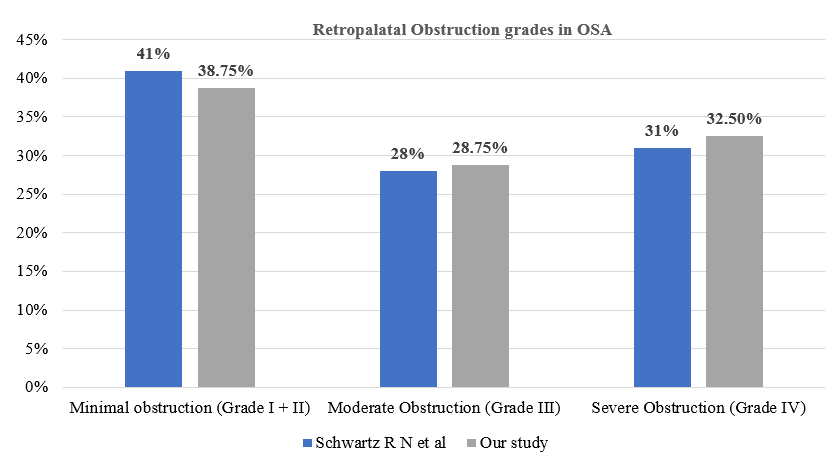
Distribution of retropalatal obstruction by nasal endoscopy
Retropalatal obstruction was classified according to Mullers grade, where we found 10% patients had grade I (0-25%) obstruction, 28.75% patients had grade II (25-50%) and 28.75% had grade III (50-75%) obstruction. Maximum number of patients i.e. 32.5% had grade IV (75-100%) obstruction.
Nasal obstruction also had non-significant correlation with grade of OSA. P value of DNS was 0.60 whereas that of other types of nasal obstruction was 0.85. (Figure 8)
Correlation with Retropalatal obstruction was significantly high with severity of OSA with P value <0.0001. (Figure 8)
Table 1
Correlation Between Severity of OSA & types of nasal obstruction by nasal endoscopy
Discussion
Obstructive Sleep Apnoea is a prevalent disease entity that has become common place over the past few decades.11 Treatment of OSA with Continuous Positive Airway Pressure Therapy (CPAP) is considered the first line therapy, but the long-term compliance is only about 40%, often because of nasal obstruction. Once treated it has been shown to reduce CPAP requirement and improve compliance with CPAP. 12
Studies suggest that the prevalence of OSA increases with age independent of other risk factors.13 Also, the increase in the OSA may be due to generalized age-related decrease in the size of upper airway lumen in older people.14 Mean age of study done by Kevin J Reichmuth15 et al was closest to present study i.e. 49 years whereas in a study done by Friedman M16 et al, it was 34 years. In our study it was found to be 54 years. Lee S J17 et al and Torre C18 et al found it to be 42 years and Chung K F 19 found it to be 44 years.
The sex ratio in present study was 2.3:1 which is close to the study done by Friedman M14 et al i.e. 1.58:1. But in a study done by Chung K F19 it was quite high i.e. 9:1. Lee S J et al17 found it to be 5.4:1. (GRAPH 13) Research study has almost repeatedly and consistently confirmed that OSA is more common in men than women.13, 14 It is believed that inherent differences in fat distribution, length and collapsibility of the upper airway, neurochemical control mechanisms, arousal response, and sex hormones all contribute to the disparity in prevalence between genders.20
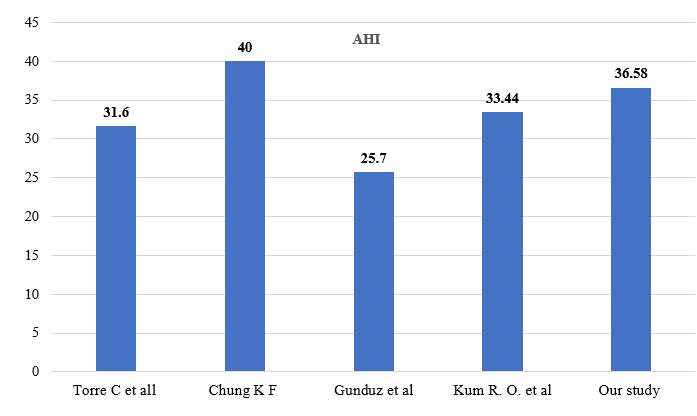
Majority of patients in our study were diagnosed to have Severe OSA (AHI > 30) and mean AHI was found to be 36.58. In a study done by Chung K F,19 the mean AHI was 40 whereas Gunduz C et al21 found it to be 25.7. Mean AHI of studies done by Torre C et al18 and Kum R O et al22 was similar to ours i.e. 31.6 and 33.44 respectively. (GRAPH 4)
Nasal obstruction is an important factor in OSA and we found it to be present in 49 out of 80 patients, i.e. 61.25%, in our study where 42 patients had deviated nasal septum, 4 had CRS with Nasal polyposis and 3 had Concha bullosa. In a study done by Torre C et al18 73 out of 274 patients were found to have nasal obstruction where 55 patients had isolated posterior septal deviation and 5 patients had combined anterior and posterior deviation. 11 patients had nasal polyposis. CRS without nasal polyposis was found in 7 out of 80 patients in our study whereas Torre C et al18 found it in 2 out of 274 patients. Mucosal inflammation was quite significant i.e. 36 out of 80 whereas Torre C et al18 found it in only 2 out of 274 patients. In a study done in 8 patients with OSA by Gregorio M G et al23 6 out of 8 (75%) patients had conchae hypertrophy and 4 out of 8 (50%) had nasal septum deviation. (GRAPH 5)
Nasal obstruction can be a result of structural abnormalities or inflammatory mucosal disease.17 There is extensive evidence that nasal obstruction not only decreases quality of life, but that it also contributes to snoring, plays an important role in pathophysiologic mechanisms leading to OSA, and represents an obstacle for effective treatment with CPAP therapy in OSA patients.7
Nasal obstruction leads to oral breathing and thus decreased hypopharyngeal airspace and increased airway resistance, exacerbating OSA.16
Oral breathing resulting from nasal obstruction may often lead to a closed cycle where nasal respiration ends up becoming worse due to profound anatomic derangement. Continuous oral breathing often leads to transverse maxillary deficiency that deepens the palatal arch. The high arched palate may compress the septum in a cranio-caudal orientation, thus resulting in a displaced septum.24 Over 70% patients with Chronic Rhinosinusitis (CRS) report poor sleep quality.25
But nasal obstruction alone cannot be responsible for OSA and multiple sites of airway obstruction are seen in moderate/severe OSA. These patients are chronic mouth breathers, and obstructing the nasal airway has little impact on their respiratory function. 26
In this study, the significance of nasal obstruction on pathophysiology of OSA and its impact on severity of OSA was found to be not significant.
The grades of retropalatal obstruction found in our study group was comparable to that found by Schwartz R N et al27 as Mild obstruction (Mullers grade I and II) 38.75% and 41%, Moderate obstruction (Mullers grade III) 28.75% and 28% and Severe obstruction (Mullers grade IV) 32.5% and 31% respectively(GRAPH 6). Thong and Pang28 reported that Muller’s maneuver findings were in correlation with AHI, and the maneuver can be used for determining patients with OSAS and can guide the treatment. Our study findings were consistent with this and correlation of retropalatal obstruction with AHI was found to be highly significant (P value= <0.0001).
Conclusion
The one-year incidence of Nasal and Nasopharyngeal obstruction in patients with abnormal polysomnography found in our study is 0.67 per 1000 population. However none of the patients in our study had any significant nasopharyngeal pathology. Nasal examination gives a primary idea about type of nasal obstruction in a patient presenting with abnormal polysomnography. Nasal endoscopy is essential to determine exact level of nasal & nasopharyngeal obstruction in patients with abnormal polysomnography. Nasal obstruction is an important, but not a significant factor in determining the severity of OSA. The most common cause of Nasal obstruction in our study was found to be Nasal congestion followed by Isolated posterior DNS. There is a poor correlation between levels of nasal obstruction and degree of obstructive sleep apnoea. There is a strong correlation between grades of retropalatal obstruction and degree of obstructive sleep apnoea. Nasal and Nasopharyngeal obstruction predict the occurrence of OSA in an adult individual. Nasal obstruction leading to Obstructive Sleep Apnoea has a significant impact on Quality of Life.