- Visibility 409 Views
- Downloads 170 Downloads
- Permissions
- DOI 10.18231/j.ijashnb.2022.015
-
CrossMark
- Citation
Variable’s of COGS analysis for Orthognathic surgery based on preferences of two specialists- A perspective based study
- Author Details:
-
Parveen Akhtar Lone *
-
Faisal Arshad
-
Jasbinder Kumar
-
Sabiha Parwaiz
Abstract
Introduction: Cephalometric analysis for Ortho-Gnathic Surgery (COGS) is the most commonly used analysis for diagnosing and treatment planning of an orthognathic case. This analysis consists of 37 parameters under 7 subheading which covers cranial, skeletal, dental, facial parameters. While performing this analysis it becomes very cumbersome for an oral surgeon and orthodontist to discuss the case with all the parameters in mind. So this study was done to determine the parameters of preference for an Oral surgeon and Orthodontist respectively.
Materials and Methods: 20 Oral surgeons and Orthodontist with 2 years of experience were selected for this study. The selection was done randomly by selecting the specialist through online list. A preferential form consisting of all the parameters of COGS analysis with three preference for each parameter-1): Important, 2): Slightly important and 3): Not so important, were distributed to both the specialists. The forms were collected and the data was tested statistically.
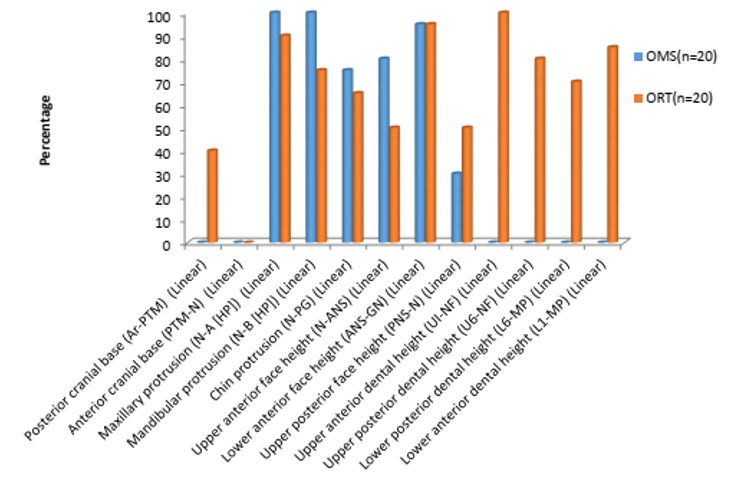
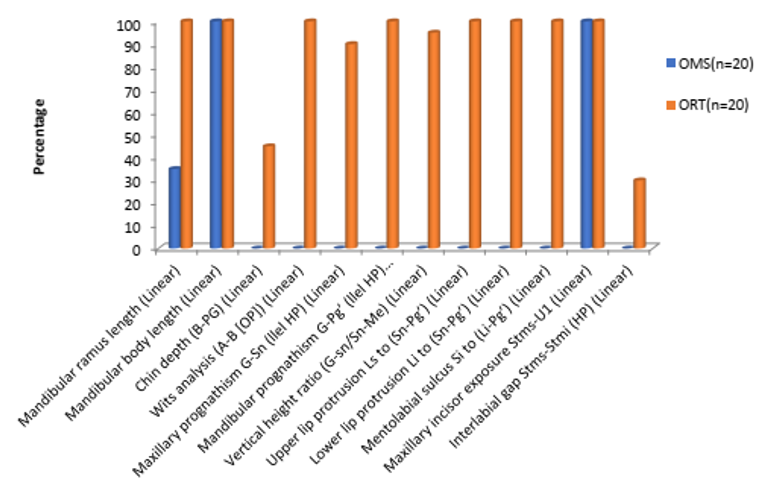
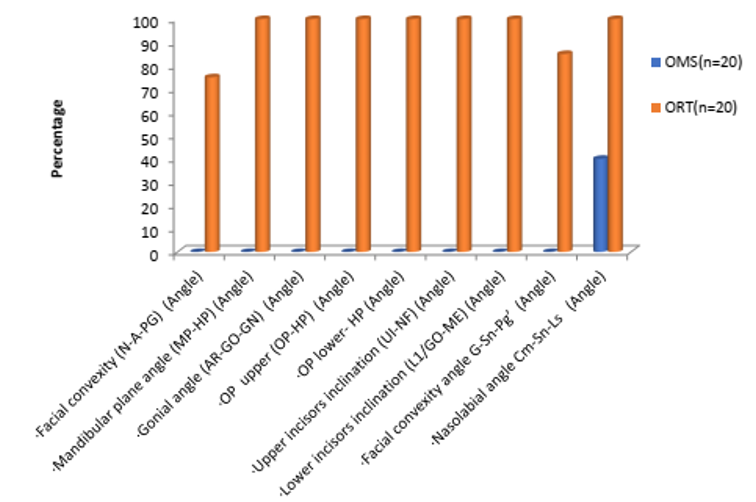
Results: Percentage wise preference was determined for various parameters. Majority of Oral and maxillofacial surgeons marked skeletal parameter as important while Orthodontist marked soft tissue as important. There was mutual agreement of preference in various parameters: Anterior cranial base (Ptm-N), Lower anterior face height (Ans-Gn), Upper posterior face height (PNS-N) which was statistically significant. Linear, angular, ratio measurement were preferred differently by oral surgeons and Orthodontists.
Conclusion: Skeletal measurements were preferred by oral surgeons followed by soft tissue & dental relationship, while as Orthodontists preferred Soft tissue, dental measurements followed by skeletal parameters.Cranial base measurements were not so marked as Ist preference by both the specialists.
Introduction
Cephalometric radiology was introduced in orthodontics in the 1930’s but it gained wider acceptance in practical application during last 20 yrs.[1] Cephalometric norms are used for guiding the clinician during diagnosis & treatment planning especially in orthognathic surgical cases to identify skeletal dysgnathia & facial soft tissue disharmony by comparing with normative values.[2] It is important for clinician to predict soft tissue changes resulting from hard tissue changes & the successful treatment of orthognathic surgical treatment depends on careful diagnosis. Literature has reported many studies which have attempted to evaluate the relation between hard tissue surgery & its effects on soft tissue. [3] Some studies have reported that clinician are more sensitive to certain profile aspect than patient & vice versa. Certain specific areas crucial to patient may not be actually crucial to clinician. [4] There are Various cephalometric analysis proposed by many authors based on hard tissue references with paradigm shift to soft tissues for orthognathic surgical cases which include: for COGS Dipaolo's Quadrilateral Analysis, Arnett's Soft Tissue Cephalometric Analysis (STCA). [5], [6], [7]
Population of adults seeking orthodontic treatment requiring orthognathic surgery are increasing day by day. For diagnosing and formulating treatment plan of an orthognathic surgical case, analysis of facial, skeletal, and dental problems is a must. For this reason, a specialized cephalometric appraisal system called COGS concerning the hard tissue and soft tissue of the face had been developed by Burstone et al.,[8] while dealing with orthognathic cases a team of specialists work in tandem which include Oral surgeon, Orthodontist, Anesthetist, Craniomaxillofacial surgeon, Neurosurgeon.
Cephalometric for orthognathic surgery analysis (COGS) developed by Burstone [8] is very popular and is commonly done cephalometric tracing for orthognathic cases. COGS analysis is a vast analysis and requires a good amount of time to analyze as it comprises of 37 parameters under seven headings which includes parameters related to: cranial bases, horizontal skeletal, vertical skeletal and dental lines and angles, Maxilla mandible relation, dental, facial form, lip position and form. These parameters are in linear, angular and ratio measurements. Though there are certain parameters which hold more importance for an oral surgeon and some for an orthodontist. An oral surgeon usually eyeballs on certain parameters to get the overall view of the case and understand the actual area of fault. While, an orthodontist considers some other parameters more important keeping in view the decompensation (reverse orthodontics), settling and finishing procedures to be performed in an orthognathic case.
The perception of facial profile differs between patients, dental professionals & peers, also the complexity of assessing orthognathic surgical treatment outcome definition differing of facial attractiveness & beauty by patient & clinician. [9], [10], [11] There is no such study done before to assess what variables are preferred from an oral surgeon and Orthodontist point of view respectively while dealing with an orthognathic case. So to our curiosity and interest we intended to perform this study to assess the preferential choice of variables for Oral surgeon and orthodontist with regard to various variables of cephalometric for orthognathic surgery analysis (COGS) developed by Burstone.
Materials and Methods
A preferential form was prepared consisting of all parameters of Burstone’s Cephalometric Analysis for Orthognathic Surgery (COGS) [11] under 7 heading and total of 37 parameters in one column. Three preferences were given for each parameter:
Preference 1 - Important parameter.
Twenty Oral and Maxillofacial surgeons and twenty Orthodontists with 2 years experience after post graduation were selected randomly for participation in this study. All the forms were sent through speed post, email and whatsapp mode and online questionnaire platform. All the participants were briefed about the study in the preference sheet (Figure 1) and asked to tick the parameter according to their preference while deciding a case of orthognathic surgery All the returned sheets were collected and data was tabulated in the excel sheet and sent for statistical analysis.
Preference sheet
Topic
This preference sheet is to know the preference of Oral surgeons and Orthodontists with regard to various variables/ parameters of Burstone Analysis (COGS) for diagnosing and treatment plan of Orthognathic surgeries.
Preference scale from 1 to 3
Tick mark ( √) the appropriate section depending upon your personal preference of parameter for diagnosing and formulating treatment plan for an Orthognathic case
|
S.No. |
Variables /Parameter |
Preference 1 Important Parameter |
Preference 2 Slightly important parameter |
Preference 3 Not so important |
|
Cranial base |
|
|
|
|
|
1 |
Posterior cranial base (Ar-PTM) (Linear) |
|
|
|
|
2 |
Anterior cranial base (PTM-N) (Linear) |
|
|
|
|
Horizontal (skeletal relation) |
|
|
|
|
|
3 |
Facial convexity (N-A-PG) (Angle) |
|
|
|
|
4 |
Maxillary protrusion (N-A [HP]) (Linear) |
|
|
|
|
5 |
Mandibular protrusion (N-B [HP]) (Linear) |
|
|
|
|
6 |
Chin protrusion (N-PG) (Linear) |
|
|
|
|
Vertical (skeletal and dental relation ) |
|
|
|
|
|
7 |
Upper anterior face height (N-ANS) (Linear) |
|
|
|
|
8 |
Lower anterior face height (ANS-GN) (Linear) |
|
|
|
|
9 |
Upper posterior face height (PNS-N) (Linear) |
|
|
|
|
10 |
Mandibular plane angle (MP-HP) (Angle) |
|
|
|
|
11 |
Upper anterior dental height (UI-NF) (Linear) |
|
|
|
|
12 |
Upper posterior dental height (U6-NF) (Linear) |
|
|
|
|
13 |
Lower posterior dental height (L6-MP) (Linear) |
|
|
|
|
14 |
Lower anterior dental height (L1-MP) (Linear) |
|
|
|
|
Maxilla and mandible |
|
|
|
|
|
15 |
Maxillary length (PNS-ANS) (Linear) |
|
|
|
|
16 |
Mandibular ramus length (Linear) |
|
|
|
|
17 |
Mandibular body length (Linear) |
|
|
|
|
18 |
Chin depth (B-PG) (Linear) |
|
|
|
|
19 |
Gonial angle (AR-GO-GN) (Angle) |
|
|
|
|
Dental relationships |
|
|
|
|
|
20 |
OP upper (OP-HP) (Angle) |
|
|
|
|
21 |
OP lower- HP (Angle) |
|
|
|
|
22 |
Upper incisors inclination (UI-NF) (Angle) |
|
|
|
|
23 |
Lower incisors inclination (L1/GO-ME) (Angle) |
|
|
|
|
24 |
Wits analysis (A-B [OP]) (Linear) |
|
|
|
|
|
Preference 1 Important Parameter |
Preference 2 Slightly important parameter |
Preference 3 Not so important |
|
|
Facial form |
|
|
|
|
|
25 |
Facial convexity angle G Sn Pg’ (Angle) |
|
|
|
|
26 |
Maxillary prognathism G-Sn (llel HP) (Linear) |
|
|
|
|
27 |
Mandibular prognathism G Pg’ (llel HP) (Linear) |
|
|
|
|
28 |
Vertical height ratio (G-sn/Sn-Me) (Linear) |
|
|
|
|
29 |
L face ht-depth ratio (Ratio) |
|
|
|
|
30 |
L face-Throat angle (Ratio) |
|
|
|
|
Lip position and form |
|
|
|
|
|
31 |
Nasolabial angle Cm-Sn-Ls (Angle) |
|
|
|
|
32 |
Upper lip protrusion Ls to (Sn Pg’) (Linear) |
|
|
|
|
33 |
Lower lip protrusion Li to (Sn Pg’) (Linear) |
|
|
|
|
34 |
Mentolabial sulcus Si to (Li Pg’) (Linear) |
|
|
|
|
35 |
Vertical lip-chin (Ratio) |
|
|
|
|
36 |
Maxillary incisor exposure Stms-U1 (Linear) |
|
|
|
|
37 |
Interlabial gap Stms-Stmi (HP) (Linear) |
|
|
|
Statistical methods
The data derived was qualitative in nature. The statistical software SPSS 22.0 ver 3.2.2 were used for the analysis of the data. Microsoft word and excel sheets have been used to generate graphs, tables etc. Descriptive and inferential statistical analysis has been carried out in the present study.
Results
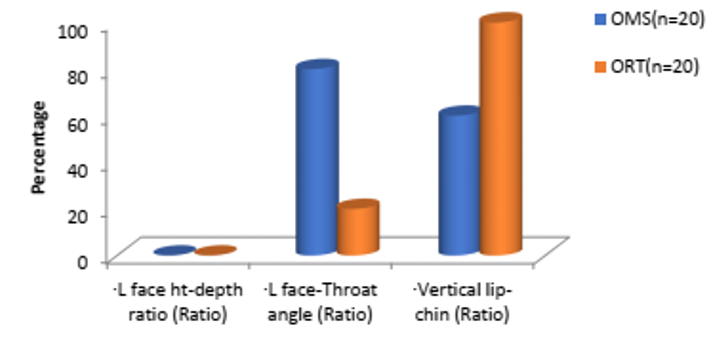
The results showed the percentage wise preference of the parameters/ variables of COGS analysis by two specialists- Oral surgeons and Orthodontists. 75% preference was considered as the majority among the three preferences.
The parameters/variables preferred as important, by majority (75%) of Oral surgeons were
Maxillary protrusion (N-A [HP] (Linear 20(100%
Mandibular protrusion (N-B [HP] (Linear 20(100%
Chin protrusion (N-PG (Linear 15(75%
Upper anterior face height (N-ANS (Linear 16(80%
Lower anterior face height (ANS-GN (Linear 19(95%
Maxillary length (PNS-ANS (Linear 20(100%
Mandibular body length (Linear 20(100%
Maxillary incisor exposure Stms-U1 (Linear 20(100%
Face-Throat (Angle 16(80%)
The parameters/variables preferred as important by majority (75%) of Orthodontists were
All parameters in vertical skeletal and dental except, upper. anterior face height, upper posterior face height and lower. posterior dental height.
All parameters in horizontal skeletal lines except chin protrusion.
All parameters in Maxilla and Mandible relation except chin depth.
All parameters in horizontal skeletal relation.
All parameters in dental relationship were marked important (100%).
All parameters in facial form except lower face height-depth ratio and lower face throat angle.
All parameters in lip position and form except interlabial gap.
The parameters/variables Equally not preferred as important parameter by both the specialist
Face ht-depth ratio (Ratio (0%).
Anterior cranial base (PTMN (Linear (0%)
Linear variables were marked as important parameter by majority of oral surgeons followed by ratio variables and angular variable.
Linear, ratio and angular variables were equally marked important by orthodontists,
Skeletal measurements were preferred by oral and maxillofacial surgeons followed by soft tissue & dental relationship form, while as Orthodontists preferred Soft tissue, dental measurements followed by skeletal parameters. Cranial base measurements were not so marked as 1st preference by both the specialists.
One ratio of L face-Throat angle (Ratio) was marked important parameter by (80%) of Oral & Maxillofacial surgeon than Orthodontists (20%),
|
Variable / Parameters |
N |
Spearman R |
t-value |
p-value |
|
1.Posterior cranial base (Ar-PTM) (Linear) |
20 |
0.1021 |
0.4353 |
0.6685 |
|
2.Anterior cranial base (PTM-N) (Linear) |
20 |
0.4644 |
2.2249 |
0.0391* |
|
3.Facial convexity (N-A-PG) (Angle) |
20 |
- |
- |
- |
|
4.Maxillary protrusion (N-A [HP]) (Linear) |
20 |
- |
- |
- |
|
5.Mandibular protrusion (N-B [HP]) (Linear) |
20 |
- |
- |
- |
|
6.Chin protrusion (N-PG) (Linear) |
20 |
-0.1816 |
-0.7833 |
0.4436 |
|
7.Upper anterior face height (N-ANS) (Linear) |
20 |
0.0000 |
0.0000 |
1.0000 |
|
8.Lower anterior face height (ANS-GN) (Linear) |
20 |
0.6882 |
4.0249 |
0.0008* |
|
9.Upper posterior face height (PNS-N) (Linear) |
20 |
0.4364 |
2.0580 |
0.0544 |
|
10. Mandibular plane angle (MP-HP) (Angle) |
20 |
- |
- |
- |
|
11.Upper anterior dental height (UI-NF) (Linear) |
20 |
- |
- |
- |
|
12.Upper posterior dental height (U6-NF) (Linear) |
20 |
0.3669 |
1.6733 |
0.1116 |
|
13.Lower posterior dental height (L6-MP) (Linear) |
20 |
0.4286 |
2.0125 |
0.0594 |
|
14.Lower anterior dental height (L1-MP) (Linear) |
20 |
- |
- |
- |
|
15.Maxillary length (PNS-ANS) (Linear) |
20 |
- |
- |
- |
|
16.Mandibular ramus length (Linear) |
20 |
- |
- |
- |
|
17.Mandibular body length (Linear) |
20 |
- |
- |
- |
|
18.Chin depth (B-PG) (Linear) |
20 |
0.0503 |
0.2135 |
0.8334 |
|
19.Gonial angle (AR-GO-GN) (Angle) |
20 |
- |
- |
- |
|
20.OP upper (OP-HP) (Angle) |
20 |
- |
- |
- |
|
21.OP lower- HP (Angle) |
20 |
- |
- |
- |
|
22.Upper incisors inclination (UI-NF) (Angle) |
20 |
- |
- |
- |
|
23.Lower incisors inclination (L1/GO-ME) (Angle) |
20 |
- |
- |
- |
|
24.Wits analysis (A-B [OP]) (Linear) |
20 |
- |
- |
- |
|
25.Facial convexity angle G Sn Pg' (Angle) |
20 |
0.2100 |
0.9115 |
0.3741 |
|
26.Maxillary prognathism G-Sn (llel HP) (Linear) |
20 |
-0.4543 |
-2.1633 |
0.0442* |
|
27.Mandibular prognathism G Pg' (llel HP) (Linear) |
20 |
- |
- |
- |
|
28.Vertical height ratio (G-sn/Sn-Me) (Linear) |
20 |
-0.3126 |
-1.3964 |
0.1796 |
|
29.L face ht-depth ratio (Ratio) |
20 |
- |
- |
- |
|
30.L face-Throat angle (Ratio) |
20 |
-0.0481 |
-0.2044 |
0.8404 |
|
31.Nasolabial angle Cm-Sn-Ls (Angle) |
20 |
- |
- |
- |
|
32.Upper lip protrusion Ls to (Sn Pg') (Linear) |
20 |
- |
- |
- |
|
33.Lower lip protrusion Li to (Sn Pg') (Linear) |
20 |
- |
- |
- |
|
34.Mentolabial sulcus Si to (Li Pg') (Linear) |
20 |
- |
- |
- |
|
35.Vertical lip-chin (Ratio) |
20 |
- |
- |
- |
|
36.Maxillary incisor exposure Stms-U1 (Linear) |
20 |
- |
- |
- |
|
37.Interlabial gap Stms-Stmi (HP) (Linear) |
20 |
0.0306 |
0.1297 |
0.8982 |
|
Parameters |
Agreement |
Kappa |
Z-value |
P-value |
|
1.Posterior cranial base (Ar-PTM) (Linear) |
40.00% |
0.0000 |
0.0000 |
0.5000 |
|
2.Anterior cranial base (PTM-N) (Linear) |
70.00% |
0.3548 |
2.0800 |
0.0189* |
|
3.Facial convexity (N-A-PG) (Angle) |
12.50% |
0.0000 |
- |
- |
|
4.Maxillary protrusion (N-A [HP]) (Linear) |
90.00% |
0.0000 |
- |
- |
|
5.Mandibular protrusion (N-B [HP]) (Linear) |
75.00% |
0.0000 |
- |
- |
|
6.Chin protrusion (N-PG) (Linear) |
50.00% |
-0.1765 |
-0.8100 |
0.7916 |
|
7.Upper anterior face height (N-ANS) (Linear) |
50.00% |
0.0000 |
0.0000 |
0.5000 |
|
8.Lower anterior face height (ANS-GN) (Linear) |
95.00% |
0.6429 |
3.0800 |
0.0010* |
|
9.Upper posterior face height (PNS-N) (Linear) |
70.00% |
0.4000 |
1.9500 |
0.0255* |
|
10. Mandibular plane angle (MP-HP) (Angle) |
17.50% |
0.0000 |
0.0000 |
0.5000 |
|
11.Upper anterior dental height (UI-NF) (Linear) |
7.50% |
0.0000 |
- |
- |
|
12.Upper posterior dental height (U6-NF) (Linear) |
27.50% |
0.0000 |
0.0000 |
0.5000 |
|
13.Lower posterior dental height (L6-MP) (Linear) |
30.00% |
0.0000 |
- |
- |
|
14.Lower anterior dental height (L1-MP) (Linear) |
7.50% |
0.0000 |
- |
- |
|
15.Maxillary length (PNS-ANS) (Linear) |
- |
- |
- |
- |
|
16.Mandibular ramus length (Linear) |
35.00% |
0.0000 |
0.0000 |
0.5000 |
|
17.Mandibular body length (Linear) |
- |
- |
- |
- |
|
18.Chin depth (B-PG) (Linear) |
37.50% |
0.0000 |
- |
- |
|
19.Gonial angle (AR-GO-GN) (Angle) |
5.00% |
0.0000 |
0.0000 |
0.5000 |
|
20.OP upper (OP-HP) (Angle) |
7.50% |
0.0000 |
- |
- |
|
21.OP lower- HP (Angle) |
7.50% |
0.0000 |
- |
- |
|
22.Upper incisors inclination (UI-NF) (Angle) |
7.50% |
0.0000 |
- |
- |
|
23.Lower incisors inclination (L1/GO-ME) (Angle) |
7.50% |
0.0000 |
- |
- |
|
24.Wits analysis (A-B [OP]) (Linear) |
7.50% |
0.0000 |
- |
- |
|
25.Facial convexity angle G Sn Pg' (Angle) |
17.50% |
0.0000 |
0.0000 |
0.5000 |
|
26.Maxillary prognathism G-Sn (llel HP) (Linear) |
22.50% |
0.0000 |
0.0000 |
0.5000 |
|
27.Mandibular prognathism G Pg' (llel HP) (Linear) |
17.50% |
0.0000 |
0.0000 |
0.5000 |
|
28.Vertical height ratio (G-sn/Sn-Me) (Linear) |
20.00% |
0.0000 |
- |
- |
|
29.L face ht-depth ratio (Ratio) |
25.00% |
0.0000 |
- |
- |
|
30.L face-Throat angle (Ratio) |
57.50% |
0.0860 |
1.1200 |
0.1318 |
|
31.Nasolabial angle Cm-Sn-Ls (Angle) |
40.00% |
0.0000 |
- |
- |
|
32.Upper lip protrusion Ls to (Sn Pg') (Linear) |
5.00% |
0.0000 |
0.0000 |
0.5000 |
|
33.Lower lip protrusion Li to (Sn Pg') (Linear) |
5.00% |
0.0000 |
0.0000 |
0.5000 |
|
34.Mentolabial sulcus Si to (Li Pg') (Linear) |
20.00% |
0.0000 |
- |
- |
|
35.Vertical lip-chin (Ratio) |
77.50% |
0.0000 |
- |
- |
|
36.Maxillary incisor exposure Stms-U1 (Linear) |
- |
- |
- |
|
|
37.Interlabial gap Stms-Stmi (HP) (Linear) |
42.50% |
0.0000 |
- |
- |
[Figure 1], [Figure 2], [Figure 3], [Figure 4] : Variable preferrence between oral surgeons and orthodontists (preferred as important)
Discussion
A collaborative approach between the orthodontist and maxillofacial surgeon is imperative to successfully devise and execute a comprehensive treatment plan with predictable outcomes. Typically, most patients will solicit surgical evaluation based primarily on the recommendation of the treating orthodontist. The patient may present to the surgeon, having already implicitly selected a preferred treatment option based on the treatment focus of the orthodontist. [12] In diagnosis of orthognathic surgical case, the cephalometric norms play a major role. [13] Many studies [14] have used composite analysis for orthognathic surgery cases to arrive at a proper diagnosis and treatment plan for an orthognathic case.
In our study, we made an attempt to find out the variables which are of much preference to Oral surgeons and orthodontists while analyzing an orthognathic case using COGS analysis. Our study revealed that Skeletal measurements were preferred by majority of oral surgeons followed by soft tissue & dental relationship form, while as, Orthodontists preferred Soft tissue, dental measurements followed by skeletal parameters., This can be attributable to the fact that oral surgeon is more interested to know the skeletal lengths for determining as to what extent BSSO maxillary advancement and mandibular setback or Bi-jaw surgery is to be performed depending upon the case. The parameters which were preferred as 100% important were Maxillary protrusion, Mandibular protrusion, Maxillary length, Mandibular body length, Maxillary incisor exposure. These parameters help in determining the Excessive maxillary and mandibular deficiency or prognathism.
Lower anterior face height (ANS-Gn) was considered important by 95 % and Upper anterior face height (N-ANS) was considered important by 80% of oral surgeons which holds importance while dealing with cases of long face patients requiring Orthognathic surgery.
L face-Throat (Angular measurement) was considered important by 80% and Chin protrusion by 75% oral surgeons. These parameters help to assess whether, genioplasty, chin augmentation, reduction sliding in asymmetric chin is to be done. Whereas, orthodontists preferred these parameters as, slightly important parameters.
Cranial base parameters were not considered important by both Oral surgeons and Orthodontists. Since such parameters are more useful to craniomaxillofacial surgeons who have expertise in skull surgeries, especially in syndromic patients.
For Orthodontists; Soft tissue, dental measurements followed by skeletal parameters were of much preference. Linear, ratio and angular variables were equally marked important by Orthodontists. All vertical (dental and skeletal relation), Dental relationships were important parameters for majority of orthodontist because these are used to determine the extent of decompensation (reverse orthodontics) which is included in pre surgical orthodontic phase done before the Orthognathic surgery.
Limitation & Further scope
A large sample of Orthodontists and Oral surgeons with higher experience in orthognathic cases could have been included. More such studies related to other analysis like Quadrilateral analysis, Arnett analysis which are beneficial for diagnosing and formulating treatment plan of Orthognathic case can be performed and a composite analysis can be developed.
Conclusion
This study concluded that there is a varied perspective regarding the preference of COGS variables by Oral surgeons and Orthodontists. Though there was some mutual agreement also regarding some of the parameters i.e: Anterior cranial base (Ptm-N), Lower anterior face height (Ans-Gn), Upper posterior face height (PNS-N).
Skeletal Variables & linear measurements are preferred as important by majority of Oral surgeons. Whereas, for majority of Orthodontist, soft tissue, dental and skeletal are preferred as important, as well as, equal preference was given to linear, angular and ratio measurements.
This study was aimed to determine the perspective about the variables of COGS analysis, as to which variables are preferred as: 1) Important, 2) Slightly important and 3) Not important for oral surgeon and Orthodontists respectively. COGS analysis is an extensive one and all parameters hold significance. This short study made an attempt to know which parameters are eyeballing for an oral surgeon and orthodontist in diagnosing an orthognathic surgical case and to arrive at an immediate treatment plan for an Orthognathic case reporting in a busy OPD.
Conflict of Interest
The authors declare no relevant conflicts of interest.
Source of Funding
None.
References
- Rakosi T, Jonas I, Graber TM. Colour atlas of dental medicine Orthodontic diagnosis. . 1993. [Google Scholar]
- Flynn T, Ambrogio R, Zeichner S. Cephalometric norms for orthognathic surgery in black American adults. J Oral Maxillofac Surg. 1989;47(1):30-9. [Google Scholar] [Crossref]
- Chew M. Soft and hard tissue changes after bimaxillary surgery in Chinese Class III patients. Angle Orthod. 2005;75(6):959-63. [Google Scholar]
- Wilmot J, Barber H, Chou D, Vig K. Associations between severity of dentofacial deformity and motivation for orthodontic-orthognathic surgery treatment. Angle Orthod. 1993;63(4):283-8. [Google Scholar] [Crossref]
- Burstone C, James R, Legan H, Murphy G, Norton L. Cephalometrics for orthognathic surgery. J of Oral Surg. 1965;36(4):269-77. [Google Scholar]
- Paolo D, Philip RJ, Maganzini C, Hirce AL, JD. The quadrilateral analysis: An individualized skeletal assessment. Am J Orthod. 1983;83(1):19-32. [Google Scholar]
- Arnett G, Jelic J, Kim J, Cummings D, Beress A, Worley C. Soft tissue cephalometric analysis: diagnosis and treatment planning of dentofacial deformity. Am J Orthod Dentofac Orthop. 1999;116(3):239-53. [Google Scholar]
- Burstone C, James R, Legan H, Murphy G, Norton L. Cephalometrics for orthognathic surgery. J Oral Surg. 1965;36(4):269-77. [Google Scholar]
- Cochrane S, Cunningham S, Hunt S. A comparison of the perception of facial profile by the general public and 3 groups of clinicians. Int J Adult Orthodon Orthognath Surg. 1999;14(4):291-5. [Google Scholar]
- Phillips C, Griffin T, Bennett E. Perception of facial attractiveness by patients, peers and professionals. Int J Adult Orthod Orthognath Surg. 1995;10(2):127-35. [Google Scholar]
- Soh J, Chew MT, Wong HB. A comparative assessment of the perception of Chinese facial profile esthetics. Am J Orthod Dentofacial Orthop. 2005;127(6):692-9. [Google Scholar] [Crossref]
- Khechoyan M. Orthognathic Surgery: General Considerations David Y. Semin Plast Surg. 2013;27(3):133-6. [Google Scholar]
- Trivedi K, Singh S, Shivamurthy D, Doshi J, Shyagali T, Patel B. Analysis of cephalometrics for orthognathic surgery: Determination of norms applicable to Rajasthani population. Natl J Maxillofac Surg. 2010;1(2):102-7. [Google Scholar] [Crossref]
- TS, HA, Gowda N. Composite Cephalometric Analysis for Orthognathic Surgery (CCAOS). Hmlyn Jr Med Surg. 2022;3(2):4-10. [Google Scholar] [Crossref]
- Abstract
- Introduction
- Materials and Methods
- Results
- The parameters/variables preferred as important, by majority (75%) of Oral surgeons were
- The parameters/variables preferred as important by majority (75%) of Orthodontists were
- The parameters/variables Equally not preferred as important parameter by both the specialist
- Discussion
- Limitation & Further scope
- Conclusion
- Conflict of Interest
- Source of Funding
- References
How to Cite This Article
Vancouver
Lone PA, Arshad F, Kumar J, Parwaiz S. Variable’s of COGS analysis for Orthognathic surgery based on preferences of two specialists- A perspective based study [Internet]. IP Indian J Anat Surg Head Neck Brain. 2022 [cited 2025 Oct 15];8(2):65-71. Available from: https://doi.org/10.18231/j.ijashnb.2022.015
APA
Lone, P. A., Arshad, F., Kumar, J., Parwaiz, S. (2022). Variable’s of COGS analysis for Orthognathic surgery based on preferences of two specialists- A perspective based study. IP Indian J Anat Surg Head Neck Brain, 8(2), 65-71. https://doi.org/10.18231/j.ijashnb.2022.015
MLA
Lone, Parveen Akhtar, Arshad, Faisal, Kumar, Jasbinder, Parwaiz, Sabiha. "Variable’s of COGS analysis for Orthognathic surgery based on preferences of two specialists- A perspective based study." IP Indian J Anat Surg Head Neck Brain, vol. 8, no. 2, 2022, pp. 65-71. https://doi.org/10.18231/j.ijashnb.2022.015
Chicago
Lone, P. A., Arshad, F., Kumar, J., Parwaiz, S.. "Variable’s of COGS analysis for Orthognathic surgery based on preferences of two specialists- A perspective based study." IP Indian J Anat Surg Head Neck Brain 8, no. 2 (2022): 65-71. https://doi.org/10.18231/j.ijashnb.2022.015
