- Visibility 38 Views
- Downloads 10 Downloads
- DOI 10.18231/j.ijashnb.2024.021
-
CrossMark
- Citation
Neglected auricular hematoma
Introduction
Auricular hematoma or hematoma auris is a collection of blood between the auricular cartilage and perichondrium.[1] Auricular hematoma usually occurs following blunt trauma to pinna, which causes blood and serum accumulation between the perichondrium and cartilage. It is most commonly seen in those who practice full contact sports such as boxing and wrestling.[2] Auricular hematoma may be on the ventral (anterior) or dorsal (posterior, near the scalp), or both sides however, its usual occurrence is seen on the ventral surface just below the helix.[3]
It usually presents as a tender, tense, and fluctuating swelling on the anterior surface of the ear, with mild to moderate throbbing pain. The most common treatment method for an auricular hematoma is drainage followed by techniques to prevent recurrence.[4] If it is not properly managed, then it can lead to complications like necrosis of pinna, perichondritis and cartilage deformity known as cauliflower ear. [5] A case of auricular hematoma with poor compliance, which lead to formation of granulation is presented in this case report.
Case Description
A 24-year male patient, resident of Jamtara, construction site worker by occupation, presented in ENT OPD, with a swelling on Right Pinna from 2 days ([Figure 1]). It was sudden in onset, gradually progressive, increased to the size of lemon in two days and was associated with mild pain. There was a history of trauma to the pinna with a falling brick over the pinna 2 days back. There was no history of fever, ear discharge, facial weakness or insect bite. The patient had no systemic illness or any history suggestive of bleeding disorders.






On examination, patient was well built, his vital signs and general physical findings were normal. Patient had a swelling, on the lateral surface of pinna, which was lying above the tragus and reaching upto the root of helix and involves both the scaphoid and triangular fossa. Tragus, antitragus and lobule region were spared. It was 3 x 3 cm in size, soft in consistency, & non tender. Fluctuation test was positive. Skin over the swelling appeared normal without any local rise in temperature. There was no swelling on the medial surface of pinna. On Otoscopic examination, there was no furuncle, discharge or debris in the external auditory canal. His tympanic membrane was intact with pearly grey colour. The results of routine laboratory tests were within normal limits.
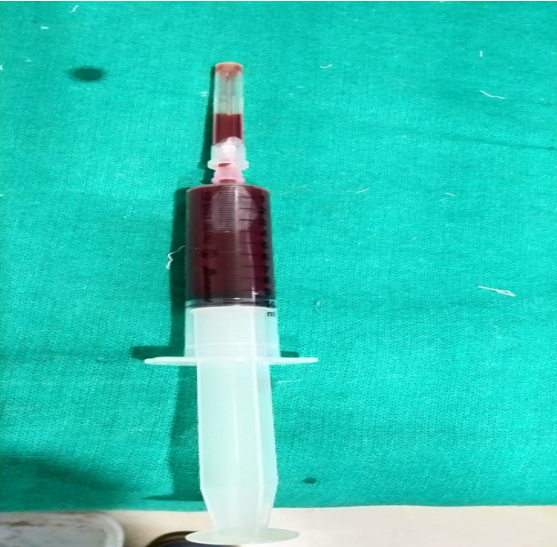
After taking the consent from the patient and following the aseptic precaution, aspiration was done under local anaesthesia. About 9ml of blood was aspirated and patient was asked to review in OPD next day ([Figure 2]). Blood was recollected when the patient came next day. Incision and drainage were done after giving local anaesthesia and around 5ml of blood was evacuated ([Figure 3]). Wound was washed with betadine and saline; mastoid dressing was done, and antibiotics were started. When the patient visited on the 3rd and 5th day, again there was collection of blood. After that button suturing was done on the pinna & patient was asked to follow up after 1 week ([Figure 4]). But the patient revisited us after 1 month and after removing the button, there was granulation tissue formation around the suture site along with serosanguineous discharge from the wound site ([Figure 5]). After proper counselling of the patient and explaining him about the complication and risk of cartilage necrosis, the patient was taken up for conservative management including wound cleaning, regular dressing, antibiotics and anti-inflammatory. This time the patient followed us regularly on alternate day basis. After a period of 10 days of regular dressing and medication, the granulation and inflammation around the wound site has subsided. ([Figure 6], [Figure 7])
Discussion
The ear is supported by a framework made up of various cartilaginous structures: the helix, antihelix, concha, tragus, and antitragus. The skin covering this cartilage is very thin, with almost no subcutaneous fat, and adheres tightly to the underlying perichondrium. The perichondrium is well-supplied with blood vessels, providing the avascular cartilage with its blood supply.[3] In the case of an auricular hematoma, blood collects in the space between the perichondrium and the cartilage, creating a mechanical barrier that obstructs the cartilage's blood supply from the perichondrium.[5] When cartilage is deprived of essential nutrients, it may experience complications such as infection, perichondritis, and necrosis. If a subperichondrial hematoma remains untreated, chondrocytes and fibroblasts from the perichondrium will invade the area and stimulate the mesenchymal cells in the perichondrium. This sequence of events can result in the chaotic development of new fibrocartilage surrounding the various cartilaginous structures, ultimately causing cauliflower ear.[6] The hematoma usually fills the space between the helix and antihelix (scapha) and may extend into the fossa triangularis or, less commonly, affect the concha or external auditory meatus. Auricular hematomas can also occur on the back of the ear or both surfaces, increasing the risk of necrosis.[7] The overlying skin may appear normal, red, or bruised.
Acute drainage is necessary for all auricular hematomas. Various treatment options have been reported, and effective management continues to be a debated topic. The most common approach involves draining the hematoma and implementing methods to prevent recurrence. Typical drainage techniques include scalpel incisions, aspiration, and the placement of materials to eliminate dead space. However, aspiration alone leads to a high rate of recurrence, often within about seven days, until the perichondrium re-adheres firmly. [4], [8]
Numerous post-procedural techniques have been described to prevent recurrence. Reported materials include tie-over and tie-through dressings, sutures, silicone splints, cotton and plaster bolsters, as well as passive and suction drainage, and clips. More recently, the use of mattress sutures, pairs of Leonard buttons, and silastic sheets has also been noted in treating auricular hematomas. While these methods help remove dead space, evenly distributing pressure across the hematoma remains a challenge. Additionally, techniques utilizing cotton bolsters for pressure application can increase the risk of postoperative infections due to wound exudate, necessitating frequent dressing changes.[9]
Non-surgical procedures, such as OK-432 intralesional injection therapy, can serve as an alternative to surgical treatment for auricular hematomas, as they are simple, safe, easy, and effective.[10] However, in our literature review, we could not find any cases reporting granulation over the pinna following incision and drainage of an auricular hematoma.
The patient being discussed in our study had been followed for the treatment of auricular hematoma with incision and drainage. However, due to the negligence on patient’s part the follow-up after button suturing was delayed. This resulted in formation of granulation over the suture site due to prolong stay of foreign material (button & sutures) at the wound site. ([Figure 5]) If in case the sutures were removed on time the complication of excessive granulation formation would not have happened. Management of the complication need to be followed in the form of conservative management with regular wound cleaning with antiseptics in addition to regular follow-up. No further negligence should be allowed in such cases.
Conclusion
It is very well known that the treatment for auricular hematoma is Incision and Drainage followed by pressure dressing to avoid recollection. However, in case of granulation tissue formation around the hematoma site because of poor compliance, the conservative management in the form of regular dressing, anti-inflammatory and antibiotics may be a helpful escape to relieve the granulation.
Source of Funding
None.
Conflict of Interest
None.
References
- M Gleeson, R Clarke. . Scott-Brown's Otorhinolaryngology: Head and Neck Surgery 2008. [Google Scholar]
- M Sellami, A Ghorbel. Traumatic auricular hematoma. . Pan Afr Med J 2017. [Google Scholar]
- M Shakeel, V Vallamkondu, R Mountain, A Hussain. Open surgical management of auricular haematoma: incision, evacuation and mattress sutures. J Laryngol Otol 2015. [Google Scholar]
- K Brickman, DZ Adams, P Akpunonu, SS Adams, SF Zohn, M Guinness. Acute management of auricular hematoma: a novel approach and retrospective review. Clin J Sport Med off J Can Acad Sport Med 2013. [Google Scholar]
- JD Greywoode, EA Pribitkin, H Krein. Management of auricular hematoma and the cauliflower ear. Fac Plast Surg 2010. [Google Scholar]
- CS Giffin. Wrestler's ear: pathophysiology and treatment. Ann Plas Surg 1992. [Google Scholar]
- K Eagles, L Fralich, JH Stevenson. Ear trauma. Clin Spor Med 2013. [Google Scholar]
- S E Jones, S Mahendran. . Interventions for acute auricular haematoma. The Cochrane database of systematic reviews 2004. [Google Scholar]
- J Haik, O Givol, R Kornhaber, M Cleary, H Ofir, M Harats. Cauliflower ear - a minimally invasive treatment method in a wrestling athlete: a case report. Int Med Case Rep J 2018. [Google Scholar]
- T Kubota, N Ohta, S Fukase, Y Kon, M Aoyagi. Treatment of auricular hematoma by OK-432. Otolaryngol Head Neck Surg 2010. [Google Scholar]
